Image: Shutterstock
Hemorrhoids, also called piles, are a common pregnancy complication that several mothers experience during pregnancy. In several cases, hemorrhoids eventually subside after delivery. However, it continues beyond pregnancy sometimes and is called postpartum hemorrhoids.
Hemorrhoids affect the anal region and make passing motions painful for many. Although they can cause severe discomfort, hemorrhoids are generally not harmful and can be treated with prompt home care and medical support.
Read this post to learn about hemorrhoids after pregnancy, including the types, symptoms, causes, treatment, and management strategies.
Key Pointers
- Postpartum hemorrhoids can result from factors such as strain during labor, hormonal changes, and pregnancy-related constipation.
- You may be prescribed certain pain-relief medications, stool softeners, or effective home remedies for mild cases of hemorrhoids after childbirth.
- They typically disappear after a few weeks, but persistent and severe cases may require surgical intervention.
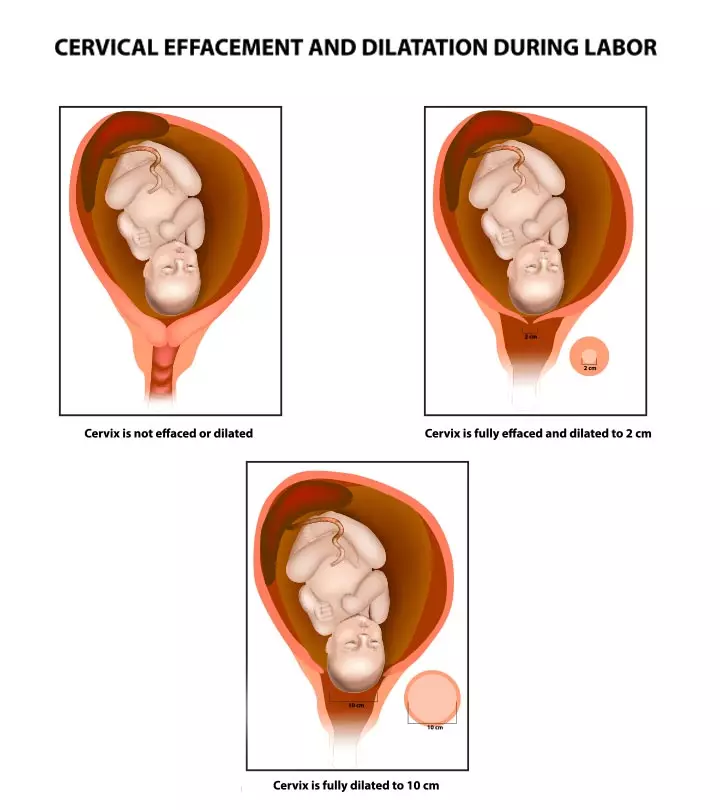
What Are Hemorrhoids (Piles)?
Hemorrhoids are swollen and engorged veins (varicose veins) in the anal region (1). They feel like a soft mass that sticks out of the anus. The size of hemorrhoids can be as small as a raisin to as big as a grape.
You are more likely to develop hemorrhoids after pregnancy if you have had them during pregnancy, and also experienced constipation. Hemorrhoids could be painful, you may even bleed while passing stools, and they can make the rectum itchy (2).
 Research finds
Research findsThe symptoms of the condition can vary based on the type of hemorrhoids you develop.
Types And Symptoms Of Postpartum Hemorrhoids
Hemorrhoids are of two types – internal and external (3).
- Internal hemorrhoids lie inside the rectum or anal canal and are not visible. They are less painful as they are only a few pain-causing nerves inside the rectum. They cause intermittent bleeding along with mucus discharge while passing stools. Some internal hemorrhoids may protrude outside the anal sphincter and appear as small grape-like lumps. In this case, these tiny hemorrhoids can be pushed back into the anus using your fingertips.
- External hemorrhoids protrude outside the anus and are easily noticeable. They are painful and cause discomfort. They also make it difficult to clean the anal region after bowel movements. In rare cases, they form blood clots (thrombosis), which is another painful condition.
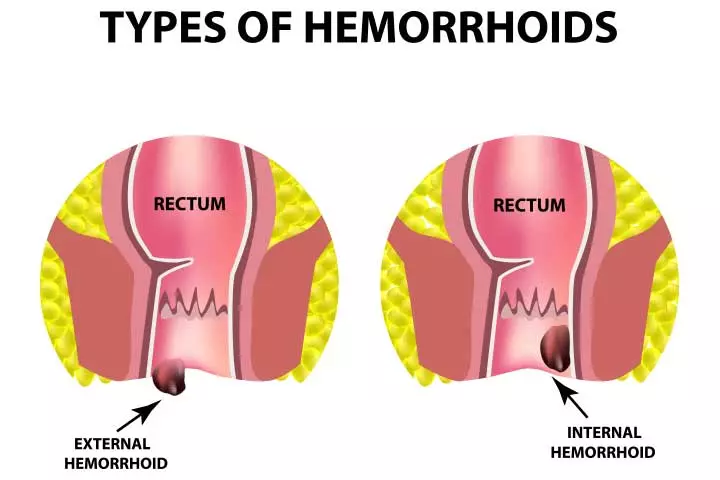
Image: Shutterstock
The common symptoms of internal and external hemorrhoids include:
- Itching and burning sensation in the anal region
- Anal pain that aggravates when you sit
- Postpartum rectal bleeding
- Pain while passing stool
- Tender mass near the anal region that can crack and bleed
The severity of symptoms increases as the disease gets worse. The frequency of symptoms determines the grade, but the symptoms remain the same across the grades. Bleeding is the most frequently reported symptom at 71.8%. Pain is next at 67.4%, followed by swelling at 55.0%. 44.1% of people report itching, while 36.2% experience prolapse. Soiling is reported in only 9.2% of cases, and fecal incontinence in 2.9%, making them not a contributor in determining the hemorrhoidal symptoms grade.

Hemorrhoidal symptoms by grade
Source: Hemorrhoidal disease and chronic venous insufficiency: Concomitance or coincidence; results of the CHORUS study (Chronic venous and Hemorrhoidal diseases evaluation and Scientific research); Clinical GastroenterologyCauses Of Postpartum Hemorrhoids

Image: IStock
Here are a few reasons why you may develop hemorrhoids after pregnancy.
- Stress on the perineum before and during delivery
- The stress of carrying a baby, and pushing it out during labor (1)
- Constipation or straining for a bowel movement
- Hormonal changes during pregnancy and childbirth affect the blood vessels that cause the veins in the legs and pelvis to swell (4)
Postpartum stress or overexertion may also lead to hemorrhoids in some individuals. Karly, a mother and blogger, says, “Resting the first few weeks after Cole was born was a challenging thing for me. I’m a busy person; I like to keep my house tidy and clean, see friends and family, walk by the beach, etc. But I needed to be sleeping when my baby was sleeping and eating, and that’s it! I felt like it was taking forever for my body to recover. I think that over-exerting myself is one of the reasons I got postpartum hemorrhoids THREE times in the first two months after giving birth (i).”
How Long Do Postpartum Hemorrhoids Last?
Based on the size, location, and severity, hemorrhoids usually take around a few days to several weeks to disappear.
Severe cases of hemorrhoids, which result in the formation of blood clots known as thrombosed hemorrhoids, can be treated using a minimally invasive procedure (5). Chronic hemorrhoids that last for months also need medical assistance.
In some mild cases, a few homecare remedial tips may help address hemorrhoids after pregnancy.
How To Manage Postpartum Hemorrhoids At Home?
Here are some of the ways to manage hemorrhoids at home (2).
- Apply ice compress (wrap some ice in a clean cloth) on the hemorrhoids and leave it for about ten minutes. This will reduce swelling and discomfort.
- Try a warm water bath. You may take a sitz bath, which is a small water tub that fits over the toilet seat. You can also soak yourself in a bathtub. Sitting on the sitz bath for about 20 minutes after each bowel movement, or for two to three times a day, could soothe the irritation. You can add Epsom salt to the water to help further reduce swelling and pain.

Image: Shutterstock
- Clean the anal region gently after each bowel movement. Use a hand-held squirt bottle and wet wipes for relief from pain.
- Use dye-free and unscented hygiene products such as menstrual pads, toilet paper, and wet wipes.
- Drink enough water and follow a post-pregnancy diet high in fiber to ease constipation and reduce discomfort.

Image: IStock
- Rest or lie down as much as possible as it takes off the pressure from your back.
- Do not control your urge to urinate because it can make the stools dry and aggravate the condition.
- Practice kegel exercises as they could improve blood circulation in the rectal region, and the perineum. They could also improve the muscle tone around the vagina.
 Quick tip
Quick tipIf these homecare measures do not provide relief from the symptoms of postpartum piles, talk to your healthcare provider for medical treatments that are safe to opt for during the lactation period.
Treatment For Postpartum Hemorrhoids
Your doctor may prescribe oral or topical medications to treat hemorrhoids. The treatments include:
- Stool softeners: They soften the stool, improve its consistency, and trigger bowel movements. Docusate sodium (Colace) and docusate calcium (Surfak) are a few such medicines you may be prescribed (6).
- Medicated wipes: They relieve itching, inflammation, and pain. Some of the most prescribed wipes are hydrocortisone, witch hazel, and lidocaine (7).
 Quick tip
Quick tip- Hemorrhoid creams and suppositories: They treat pain and inflammation of both internal and external hemorrhoids. Glycerin and bisacodyl are some frequently used suppositories to treat constipation and alleviate the symptoms of hemorrhoids (8).
- Fiber supplements: Fiber supplements include psyllium (Metamucil, Konsyl, others), methylcellulose (Citrucel) and calcium polycarbophil (FiberCon, Equalactin) (9).

Image: IStock
- Pain relievers: Tylenol (acetaminophen) or ibuprofen are recommended for temporary relief (9).
In extreme and rare cases, surgery is needed. Your obstetrician may recommend any of the following surgical treatments if necessary (10).
- Rubber band ligation: A special rubber band is tied around the base of the hemorrhoid to cut off the blood supply. The banded part then shrinks and falls off within a week or so.
- Sclerotherapy: A chemical solution is injected into the internal hemorrhoids and the surrounding area. It will affect the blood flow and shrink the hemorrhoids.
- Coagulation therapies: These treatments use infrared light or electricity to burn and remove the internal hemorrhoids.
- Hemorrhoidectomy: This traditional surgical procedure removes large hemorrhoids and prolapsing internal hemorrhoids by giving anesthesia. It is done for both internal and external hemorrhoids.
- Hemorrhoid stapling: It uses a special device to staple and removes the internal hemorrhoids.
Always consult with your healthcare provider before using any medications or treatments, especially for lactating mothers, to ensure safety for both you and your baby.
Frequently Asked Questions
1. Can postpartum hemorrhoids become permanent?
Postpartum hemorrhoids aren’t permanent. In most cases, they heal on their own within two to four weeks (11). However, in some instances, they may persist for longer. If you have hemorrhoids that don’t go away, speak to your healthcare provider.
2. Do prolapsed hemorrhoids go away after pregnancy?
Hemorrhoids that bulge out of the anus are called prolapsed hemorrhoids. They may go inside on their own, or you may have to push them back into the anus. However, if a prolapsed hemorrhoid can’t be pushed back, it must be treated surgically ( 12).
3. Can I use hemorrhoid cream while breastfeeding?
A hemorrhoid cream/ointment is applied in and around the anal area to relieve itching, swelling, and pain (13). According to experts, these creams can be safely used during pregnancy and breastfeeding (14).
4. What happens if hemorrhoids go untreated?
Most hemorrhoids go away on their own with little or no medical intervention. However, sometimes, treatment may be essential to relieve pain and discomfort. In such cases, leaving hemorrhoids untreated can worsen pain and inflammation. It may also lead to infection and other complications.
Postpartum hemorrhoids are a common issue that can occur after vaginal delivery or a c-section. Although it is more common during pregnancy, you may experience it postpartum due to natural factors accompanying the delivery process. Therefore, do not panic. Instead, work on its prevention by adopting certain lifestyle changes, such as eating fiber-rich foods and staying hydrated. However, if you still experience postpartum hemorrhoids, they may likely self-resolve. They may persist for extended periods in rare conditions and can be treated with minor medical treatments and home care.
Infographic: Can Dietary Modifications Relieve Hemorrhoids?
Dietary modifications may help to improve bowel function and reduce the incidence of constipation. You may also follow additional care such as creams and sitz baths to reduce hemorrhoids after delivery. Go through the infographic to know dietary modifications to reduce hemorrhoids in postpartum.
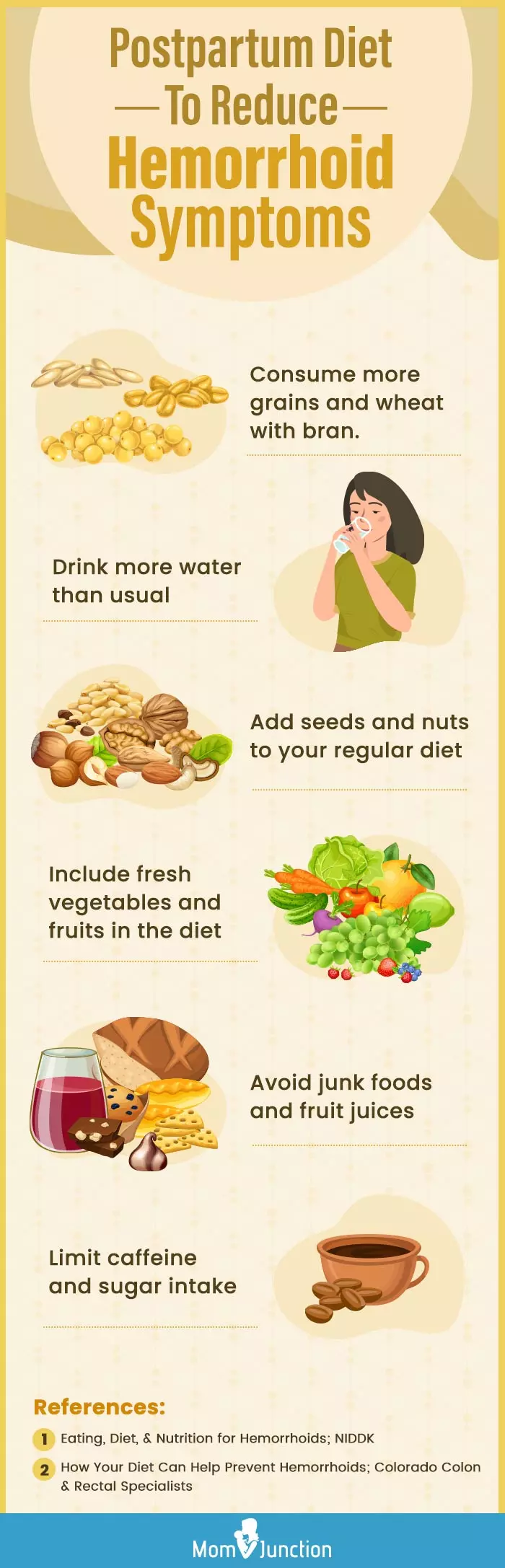
Illustration: Momjunction Design Team
Illustration: Postpartum Hemorrhoids: Types Causes Treatment And Homecare

Image: Dall·E/MomJunction Design Team
Postpartum hemorrhoids are terribly uncomfortable for a new mother. The following video provides you with a few simple tips and tricks on how to reduce pain and discomfort.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Postpartum realness.https://parthippie.wordpress.com/2019/03/01/postpartumrealness/
References
- What to Know After Having Your Baby (if you had a vaginal birth); UNM Hospitals
https://hsc.unm.edu/health/patient-care/womens-health/doc/patient-education/postpartum-vaginal-birth-english.pdf - Common Conditions; University of Rochester Medical Center
https://www.urmc.rochester.edu/ob-gyn/obstetrics/after-delivery/common-conditions - Hemorrhoids and what to do about them; Harvard Health Publishing
https://www.health.harvard.edu/diseases-and-conditions/hemorrhoids_and_what_to_do_about_them - Donna Freeborn et al.; Hemorrhoids and Varicose Veins in Pregnancy; University of Rochester Medical Center
https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=134&contentid=9 - Richard Burney; Thrombosed External Hemorrhoids; Michigan Medicine
https://www.med.umich.edu/1libr/Surgery/GenSurgery/ThrombosedHem.pdf - Stool Softeners; NIH (2018)
https://medlineplus.gov/druginfo/meds/a601113.html - Meghan Duck; Postpartum Assessment and Common Postpartum Complications: Pain management Urinary Retention & Hematoma; UCSF Benioff Children’s Hospital (2018)
https://bchsfoutreach.ucsf.edu/sites/bchsfoutreach.ucsf.edu/files/handouts/Washington%20Hospital%20Postpartum%204-2018.pdf - Meredith Portalatin and Nathaniel Winstead; Medical Management of Constipation; Clin Colon Rectal Surg (2012)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3348737/ - Treatment of Hemorrhoids; NIH (2016)
https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/treatment - Hemorrhoids What Is It; Harvard Health Publishing (2019)
https://www.health.harvard.edu/diseases-and-conditions/hemorrhoids-a-to-z - Your changing body; Allina Health
https://www.allinahealth.org/health-conditions-and-treatments/health-library/patient-education/beginnings/your-recovery-at-home/your-changing-body - Hemorrhoids: Expanded Information; American Society of Colon and Rectal Surgeons
https://fascrs.org/patients/diseases-and-conditions/a-z/hemorrhoids-expanded-version - Hemorrhoids; Medline Plus
https://medlineplus.gov/hemorrhoids.html - Over The Counter Medications During Pregnancy And Breastfeeding; University of Regina/Sask Polytechnic (2015)
https://saskhealthauthority.ca/locations_services/Services/Maternal-Newborn-Care/Documents/MedicationsandBreastfeeding.pdf - Diana Bužinskienė et al.; (2022); Perianal Diseases in Pregnancy and After Childbirth: Frequency Risk Factors Impact on Women’s Quality of Life and Treatment Methods.
https://www.frontiersin.org/journals/surgery/articles/10.3389/fsurg.2022.788823/full - Recovering from delivery.
https://kidshealth.org/en/parents/recovering-delivery.html
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Anita Gondy
Read full bio of Rebecca Malachi
Read full bio of Dr. Ritika Shah
Read full bio of Reshmi Das