Image: Shutterstock
Around one in 100 pregnant mothers have a weak cervix during pregnancy, which cannot hold the baby till the end of gestationiThe time taken for the fetus to develop in the uterus, starting from conception to birth
(1). Experts refer to such a cervix as an incompetent cervix because it opens up early during pregnancy and increases the risk of premature birth or miscarriage.
To manage this condition, an obstetric surgery called the cervical cerclage is carried out, where the cervix is stitched to help it hold the baby. Your doctor will decide whether you need the procedure or not if a cervical issue is diagnosed.
Read this post to understand more about cervical cerclage, the procedure, and the risks involved. A healthy cervix is crucial for preventing complications such as miscarriage and preterm birth. Thus, monitoring any cervical changes during pregnancy can help in the early identification and treatment of potential issues.
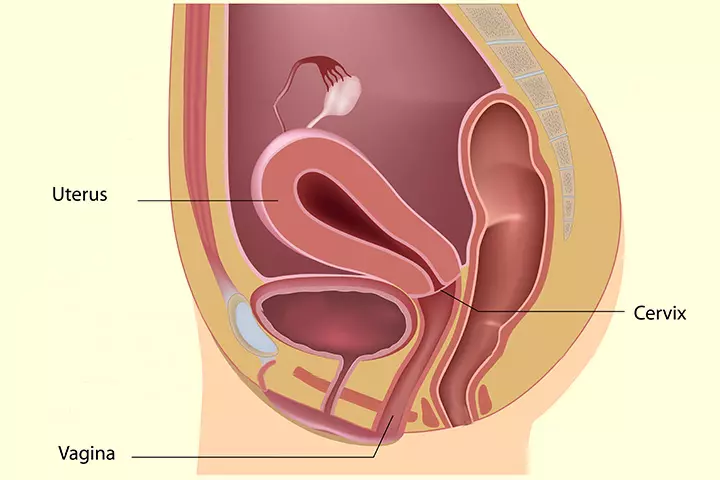
Image: Shutterstock
Key Pointers
- Surgeons perform cervical cerclage to close the cervix and prevent preterm birth.
- It is necessary when there is a risk of miscarriage, premature delivery, or pregnancy loss caused by cervical incompetence, or cervical shortening.
- The procedure is typically conducted at 12 to 14 weeks of pregnancy and may result in vaginal discharge or cramping afterward.
- Cervical cerclage can cause complications, including premature rupture of membranes, premature labor, and placental abruption.
What Is Cervical Cerclage?
Cervical cerclage or cervical suture is a surgical procedure done to prevent an incompetent cervix from opening up early during pregnancy. It is done by stitching the cervix to hold it and avoid premature delivery (1).
The procedure, which has been practiced for over 50 years, is usually done in the second trimester to hold the pregnancy until 37 weeks. In a study by multiple institutes, the survival rates after cervical emergency cerclage were 74% for overall survival, 88% for fetal survival, and 90% for neonatal survival.
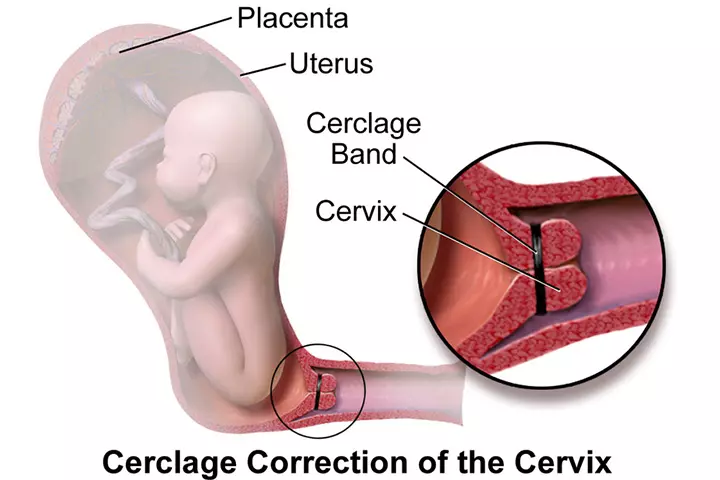
Image: Photo by BruceBlaus/CC BY-4.0
The cervical suture is done only if it is necessary and the necessity is determined by certain factors.
Why Is Cervical Cerclage Done?
The suture is done in the below cases (2) (3):
- Risk of miscarriage due to an abnormally shaped uterus or damaged cervix.
- Previous preterm labor or fetal loss in the second trimester due to cervical incompetence.
- Changes in the cervix that may lead to premature birth.
- A previous surgery or trauma to the cervix due to destructive forces or forced dilatation.
- History of inflammation or infection.
- Cervical shortening.
The above factors make you more prone to premature delivery and hence the stitch might be required. However, the procedure is not done too early in your pregnancy.
 Point to consider
Point to considerWhat Is The Right Time For Doing Cervical Cerclage?
Cervical cerclage is usually done at 12 to 14 weeks of pregnancy, i.e., before the cervical effacementiThe softening, thinning, and shortening of the cervix during the end of the pregnancy to prepare the body for labor and childbirth (1). In some cases, this procedure is done at 24 weeks but seldom after that due to the risk of amniotic saciA thin-walled sac filled with fluid that covers and protects the fetus rupture.
Some women have to undergo emergency cerclage in the later stages if the cervix has already begun to open (2 to 4cm) (3).
The procedure is carried out only if the doctor or the obstetrician diagnoses cervical issues during medical check-ups.
 Did you know?
Did you know?What Is The Preparation Process For Cervical Cerclage?
An incompetent cervix is diagnosed by the history of pregnancy losses and through an ultrasound scan. A scan helps determine the cervical dilation and short cervix (cervical length of less than 25mm).
Here is the preparation process for the procedure (4):
- A transvaginal ultrasound scan is done to check the health of the fetus.

Image: Shutterstock
- A blood test checks for any infections.
- The mother should avoid having food or water for eight hours before surgery to prevent nausea and vomiting during the surgical procedure (6).
- The mother should avoid sexual intercourse for a week before the procedure.
- Stop taking any medications.
The preparation begins once the appointment is fixed for the cerclage procedure.
What To Expect During And After The Procedure?
Cervical cerclage is carried out by giving a general, spinal, or epidural anesthesia. A special instrument called speculum is inserted into the vagina to spread the vaginal walls apart to carry out the surgery.
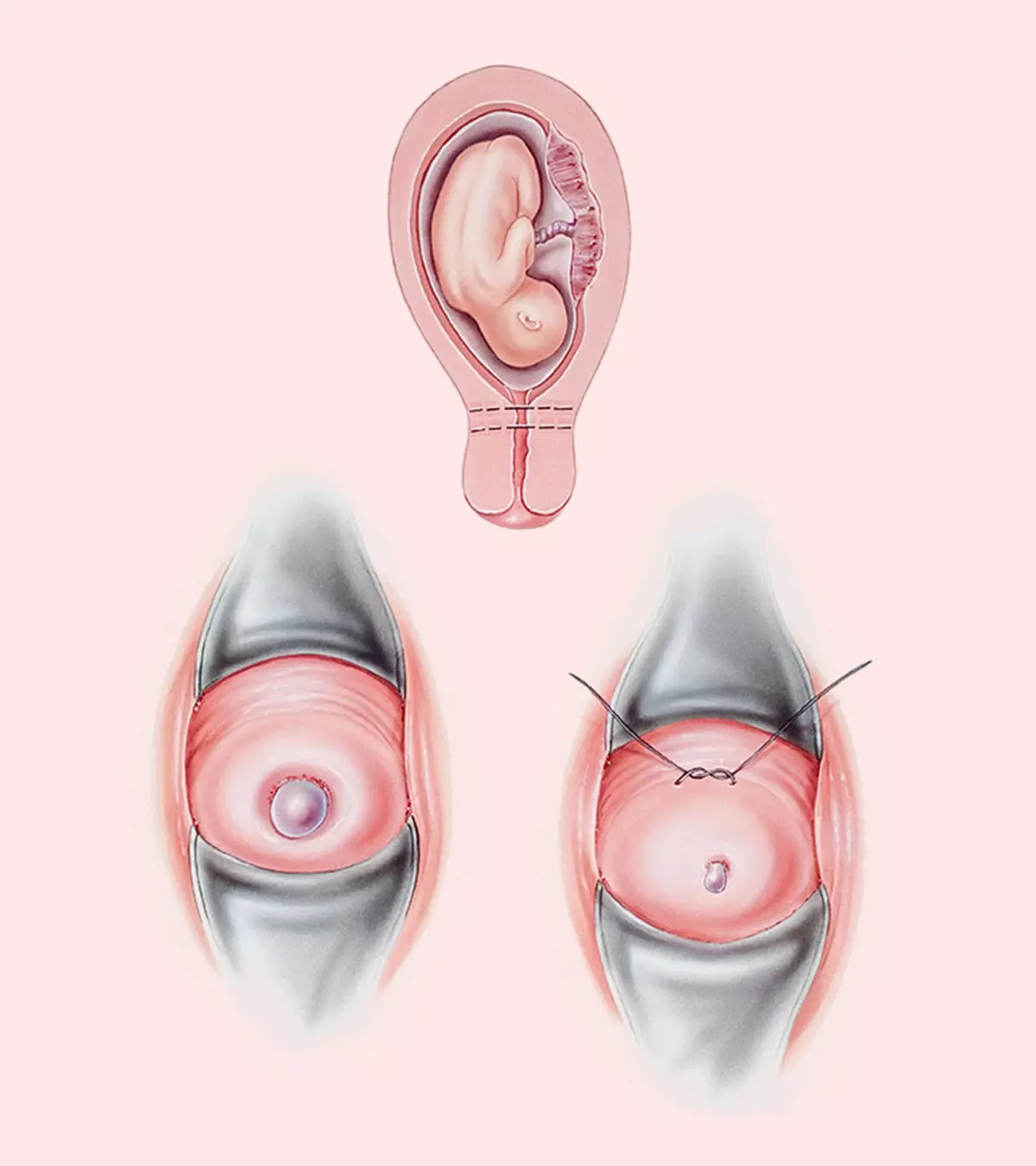
One of the three methods is used for the cerclage (4):
- Shirodkar cerclage method: The doctor will pull the vaginal wall apart to pull the cervix towards her and make an incision into it. Then she will pass a needle with tape through the incision to tie the cervix. The sutures pass through the walls of the cervix. The cerclage is made farther from the junction of the vagina and cervix. These stitches often necessitate a C-section delivery.

Image: Shutterstock
- McDonald cerclage method: The doctor uses a needle to place the stitches around the outside of the cervix, i.e., around the intravaginal segment of the cervix. The cerclage is done nearer to the junction of the cervix and vagina. These stitches are removed on reaching full term.
- Abdominal cerclage method: This is done if the cervix is too short for the above two procedures or vaginal cerclage has failed. The doctor places a tape around the cervical passage to tie it. In these cases, a C section is done for the delivery.
Laparoscopic transabdominal cerclageiSurgery to treat cervical insufficiency where the top portion of the cervix is sutured, close to where it joins the uterine body method is being preferred to the other types because it does not require hospitalization, has less post-operative pain and is quick to heal.
If incompetence of the cervix is diagnosed in the later stage then it can cause the amniotic sac to protrude through the cervix. In such cases:
- A catheter is inserted into the cervix. The balloon at the end of the catheter is inflated to close the cervix.
- Another method is to fill up the urinary bladder by inserting a catheter through the urethra. As the full bladder pushes the amniotic sac into the pelvis, the cervix is stitched.
After the procedure (aftercare) (5)
- You will be under observation for several hours to ensure that you do not show any sign of premature labor. The doctor will do an ultrasound scan to check the well-being of the fetus.
- You might experience cramps, spotting, or vaginal discharge for a few days after the surgery.
- The doctor may recommend antibiotics to fight infection and medication for pain relief.
- You may be told not to engage in physical activities or sexual intercourse for a few weeks after the surgery.
- In the follow-up visits, the doctor will check the stitch and look for any signs of preterm labor.
If you observe anything abnormal post-surgery, then call the doctor immediately.
S. Nycole Laff recounts her post-surgery experience with cervical cerclage, expressing satisfaction with the procedure. She notes, “Surgery went well. I had no contractions, and my amniotic sac remained intact– yay! I was able to get a sandwich in recovery and lots of apple juice, and about 3 hours later I could feel all of my parts and use the potty, so they let me go home. I was kept on modified bed rest and pelvic rest. The doctor also switched me from the 17P injections to a vaginal progesterone suppository that has been shown to lower cervical elasticity and help prolong the pregnancy (i).”
When To Call The Doctor?
You need to talk to your doctor if you notice any of the following symptoms (5):
- Any signs of infection along with chills or fever
- Excessive vaginal discharge, bleeding, or pain
- Cramping or contractions
- Water break
- Persistent nausea or vomiting
- If any symptom gets worsened or a new symptom is noticed
You need to take proper care of yourself and avoid any physical and mental pressure for the procedure to be successful, and the sutures to be there until they are removed.
 Be watchful
Be watchfulWhen Is Cervical Cerclage Removed?
The cerclage is usually removed at around 37 weeks or when you have preterm labor (contractions and water break) before 37 weeks of pregnancy.
The mean time between the removal of the stitch and delivery is 9.4 +/- 8.8 (mean +/- standard deviation) days (6).
A McDonald cerclage is removed at a hospital without any need for anesthesia while a transabdominal cerclage removal needs another incision in the abdomen.
What Is The Success Rate Of Cervical Cerclage?
The overall success rate of cervical cerclage in preventing preterm labor was found to be 80%. In case of women with cervical insufficiency, the McDonald procedure increased the success rate of term deliveries to 95.4%.
The rate of fetal survival after cervical cerclage was found to be 85% and premature deliveries was 18.7% (7).
Although the cerclage helps decrease the chances of preterm deliveries, we cannot overlook the pregnancy complications associated with it.
What Are The Risks Of Cervical Cerclage?

Image: Shutterstock
The risks of cervical cerclage include (4) (5) :
- Infection
- Excessive vaginal bleeding
- Damage to the cervix during surgery
- Preterm premature rupture of membranes (PPROM), when the amniotic sac breaks before 37 weeks of pregnancy
- Preterm labor
- Tearing of the cervix (cervical laceration), when labor progresses with the stitches in place
- Permanent narrowing or closure of the cervix (cervical stenosis)
- Adverse reaction to anesthesia
- Another cerclage for future pregnancies
- Inability of the cervix to dilate during normal labor
Frequently Asked Questions
1. Is normal delivery possible after cervical cerclage?
The cervical cerclage would be placed until 37 to 38 weeks of gestation. As the delivery date approaches, the doctor will remove the cerclage to initiate normal delivery (4).
2. How does the cervix change in early pregnancy?
The cervix might start to change in the early days of pregnancy. During menstruation, the cervix is present at a lower level. However, the cervix rises to a higher level in the vagina during ovulation and after conception.
3. How do I feel my cervix when pregnant?
A change in the texture of the cervix can be observed after conception. While the cervix of non-pregnant women is hard in texture, it becomes softer after conception (5). Despite the cervix being a reliable indicator of pregnancy, it is not preferred as a standard test since distinguishing a texture could be challenging.
4. What lifestyle changes can support cervical health during pregnancy?
To support your cervical health during pregnancy, focus on eating a healthy diet rich in nutrients such as folic acid, calcium, and iron, and consider taking a prenatal vitamin. Avoid alcohol, drugs, caffeine, and tobacco, and ensure you gain weight in a healthy, controlled manner throughout your pregnancy. You may engage in moderate exercise for 30 minutes a day, five days a week, and attend regular prenatal checkups to monitor both your health and your baby’s.
Cervical cerclage is performed to prevent premature delivery and other complications in women with an incompetent cervix during pregnancy. Your gynecologist may suggest you go for cervical cerclage during the second trimester of pregnancy if they find your cervix is incompetent during the routine scans. The doctor will keep you under observation for a few hours after performing the cervical cerclage procedure. If you notice any unusual pain, bleeding, or symptoms after the procedure, do not hesitate to contact your healthcare professional.
Infographic: Reasons For Undergoing Cervical Cerclage During Pregnancy
Although going through any surgical procedure when pregnant is generally not recommended, cervical cerclage is a procedure your doctor may recommend to stitch up the cervix. But why is this needed? Check out the infographic below to know the possible reasons for undergoing cervical cerclage during pregnancy.
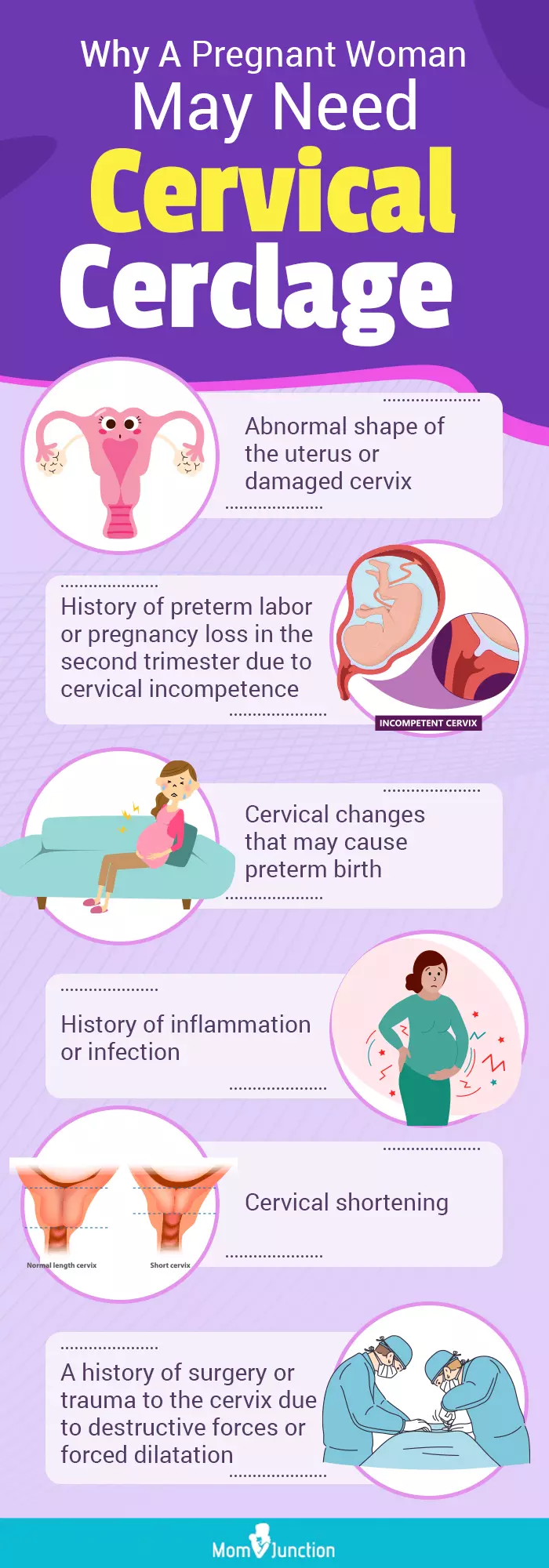
Illustration: Momjunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. 24w 5d– Lots of catching up to do… Part the first.https://spawningthoughts.wordpress.com/2012/09/13/24w-5d-lots-of-catching-up-to-do-part-the-first/
References
- Incompetent Cervix.
https://my.clevelandclinic.org/health/diseases/17912-incompetent-cervix - Danielle Abbott et al.; (2012); Cervical cerclage: A review of current evidence.
https://www.researchgate.net/publication/221833441_Cervical_cerclage_A_review_of_current_evidence - Li-Qiong Zhu et al.; (2015); Effects of Emergency Cervical Cerclage on Pregnancy Outcome: A Retrospective Study of 158 Cases.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4444177/ - Cervical Cerclage.
https://www.birthinjuryhelpcenter.org/birth-injuries/prenatal-problems/cervical-incompetence/cervical-cerclage/ - Cervical Cerclage.
https://americanpregnancy.org/healthy-pregnancy/pregnancy-complications/cervical-cerclage/ - Nathan S Fox et al.; (2009); Labor outcomes after Shirodkar cerclage.
https://pubmed.ncbi.nlm.nih.gov/19639925/ - Zakkia Khan et al.; (2015); Success Rate of Cervical Cerclage in Preventing Preterm Labour.
https://www.omicsonline.org/open-access/success-rate-of-cervical-cerclage-in-preventing-preterm-labour-2376-127X-1000176.php?aid=58436
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Shalini MA
Read full bio of Sakshi Mishra
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das