Image: ShutterStock
The placenta is a vital organ that supplies blood and nutrition to the fetus. During the third stage of labor, the body pushes it out as its work is done. However, if it doesn’t come out easily, it results in the retained placenta. This can be a serious problem that could cause life-threatening, severe infections and blood loss without prompt medical care. Keep reading as we tell you more about the causes of retained placenta, its risks factors, diagnosis, treatment, and possible complications.
Key Pointers
- Retained placenta occurs when the placenta and membranes are not expelled from the uterus within 30-60 minutes after birth.
- The woman may experience symptoms such as fever, foul-smelling discharge, persistent bleeding, severe cramps, and delayed milk production after childbirth.
- If untreated, retained placenta may result in serious complications such as excessive blood loss and infection.
- Risk factors for retained placenta include preterm labor, prolonged labor, previous uterine surgery, and stillbirth.
What Is Retained Placenta?
Image: Shutterstock
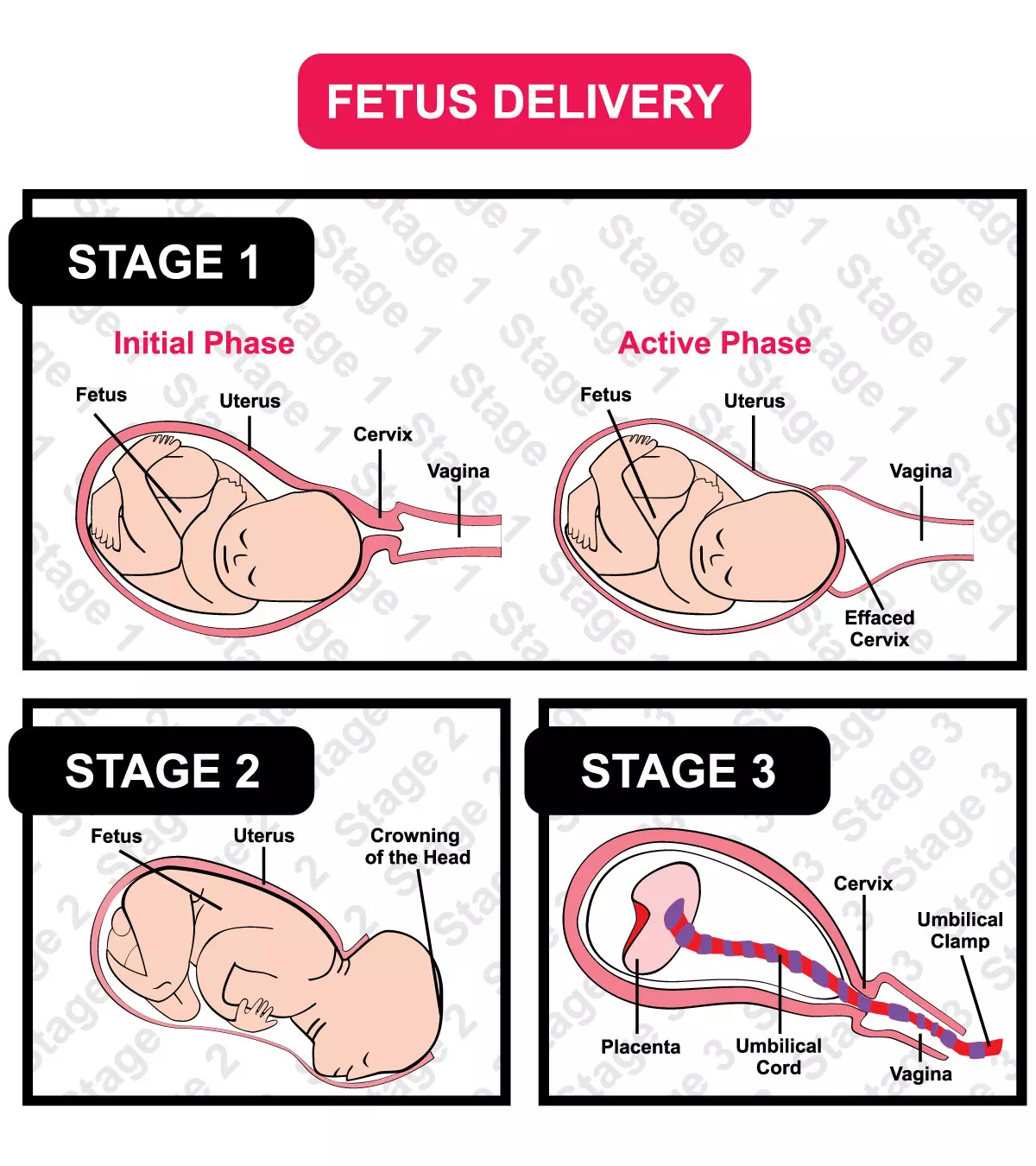
There are three vital stages of labor:
- The first stage is when you experience the contractions which dilate your cervixiThe lowest portion of the uterus that connects to the vagina to form a passage between the two organs. to prepare for childbirth (cervical dilatation up to10cm)
- Second is when your baby delivers.
- Third is when you deliver placenta and membranes, which goes on for five to 15 minutes.
Retained placenta is a condition in which you fail to expel placenta and membranes within 30 minutes of the birth of your baby. This condition is also known as retained fetal membrane or retained cleansing.
As per the US National Institute for Health and Care Excellence (NICE), the third stage is considered retained or delayed if it takes more than 30 minutes with active management, or 60 minutes with maternal effort (1).
If you leave retained placenta untreated, it can lead to life-threatening complications including excessive blood loss, infection, or sepsis.
Crystal Vargas, a mother and content creator, reflects on her encounter with retained placenta. She recalls, “I was lying there, eagerly anticipating the delivery of the placenta. As I waited, 30 minutes passed, and the doctor started giving me a strange look. Suddenly, she stood up, removed her scrubs, and left the room. I had no idea where she went, but she returned shortly, putting her scrubs back on in a hurry. Then, she urgently called out to a nurse, mentioning something about a retained placenta. I was bewildered, not understanding what that meant. As she sat back down, the nurses gathered around me, attempting to have me push, but the placenta refused to come out (i).”
What Causes A Retained Placenta?
The following are some of the main causes of retained placenta.
- Uterine Atony: The most common type of placental retention is where the uterus does not contract enough or stops contracting for the placenta to come out from the uterus (2).
- Trapped Placenta: It occurs when the placenta detaches from the uterus but gets trapped behind the closed cervix. It usually happens when the cervix begins to close before the placenta is completely removed (3). Hour-glass contracture of uterus.
- Placenta Adherens: When complete or a part of the placenta is firmly attached to the uterine wall, it is known as placental adherens. In rare cases, it happens when the part of the placenta is deeply embedded into the wall of the uterus, known as placenta accreta. It is more likely to occur when the placenta embeds itself in a previous C-section scar. If the placenta grows all over the wall of the uterus, it is known as placenta percreta.
- Maternal health conditions: Certain maternal health conditions, such as high blood pressure and diabetes, can contribute to the risk of retained placenta. These may affect uterine contractions and complicate the delivery process.
Some other rare causes include:
- Succenturiate Lobe: Retained placenta can also develop when a small piece of placenta is connected to the main part by a blood vessel that is left behind in the uterus. This blood vessel is known as a succenturiate lobe (4).
Retained Placenta Risk Factors
Image: Shutterstock
We cannot predict if any of the above cases could happen to a mother. However, certain factors increase the risk of the condition (5).
- Premature labor or giving birth before the 34th week of pregnancy.
- Induction or augmentation of labor.
- Lobulated placentaiPlacenta that is divided into several lobes by membranes. .
- Previous cases of retained placenta.
- Having more than five births previously.
- Conceiving after the age of 35.
- Giving birth to a stillborniBaby born with no signs of life (happening at or after 20 weeks of pregnancy due to various reasons). baby.
- Prolonged first or second stage of labor.
- Previous uterine surgery.
If you have any of the above risk factors, then your healthcare provider will discuss ways to manage the third stage and assist you through it.
 Things to know
Things to knowSigns And Symptoms Of Retained Placenta
When there is retained placenta in the body, you will experience symptoms a day after your delivery. They may include:
- Fever
- Foul smelling discharge containing large tissue residue
- Persistent bleeding
- Severe cramps and contractions
Image: Shutterstock
- Delay in milk production
The International Board Certified Lactation Consultant (IBCLC) Renee Kam states that the placental expulsion is the signal for breast milk production. If placenta remains inside the uterus, this signal is interrupted, and therefore the milk supply alters. Early recognition of these symptoms is vital, as untreated retained placenta can lead to severe complications. If you experience any of these signs, contact your healthcare provider immediately.
Diagnosis Of Retained Placenta
Image: Shutterstock
A careful examination by your midwife or the doctor can diagnose the retained placenta. She checks if the expelled placenta is still intact with the uterus after delivery. Even a small retained portion can be a cause of worry. Follow-up care is crucial to address any retained fragments appropriately, as they can lead to complications if left untreated.
In a few cases, your doctor may not diagnose the missing part of the placenta. But, when you begin to experience the symptoms after delivery, it signals retention.
The diagnosis includes an ultrasound scan to check for retained placental fragments in the womb. If any part is found to be retained, you will require immediate treatment to prevent complications.
Complications Of Retained Placenta
In a standard delivery, the uterus contracts to hinder all the blood vessels inside it. But, if the placental tissue is left in the uterus, it cannot contract properly, and the blood vessels continue to bleed.
If it is a managed third stage, and placenta delivery takes more than 30 minutes after the baby is out, the risk of heavy bleeding increases significantly. Excessive blood loss during the first 24 hours after delivery is called Primary Postpartum Hemorrhage (PPH) (6).
If there are still small fragments left in the uterus, it can lead to heavy bleeding even after three to seven days of delivery and infections later though it occurs in just one percent of all the births (7). This condition is called Secondary Postpartum Hemorrhage.
In addition to physical complications, the subsequent medical interventions can lead to emotional distress and anxiety. It’s essential you take care of your mental health during recovery, as the experience can be traumatic.
How You Can Separate The Placenta
If your third stage of labor is taking time, you should try to breastfeed your little one or rub your nipples so that oxytociniA chemical messenger and hormone involved in childbirth, lactation, and social bonding. hormone releases. It causes contractions in the uterus and helps in birthing the placenta and membranes (8). You should also try to change your position by turning upright so that gravity helps in expelling the placenta.
In a physiological third stage of labor, if the placental delivery does not happen within an hour, go for managed third stage. Your doctor gives an oxytocin injection for your uterus to contract. Also, your doctor will assist in pulling out the placenta.
In case the placenta doesn’t come out even after managed third stage, your doctor will give you another oxytocin injection and also inject saline into your umbilical vein to expel the placenta.
Retained Placenta Treatment
If the above doesn’t work, you may go for further treatments.
- Manual removal of placenta: Your doctor performs this either in a delivery room or operation theater. She will insert a catheter to empty the bladder, and give you intravenous antibiotics to prevent any infection. You will also get a local anesthesia, either spinal or epiduraliA type of anesthesia employed in pain management during labor and childbirth. . The practitioner will then place her hand inside the uterus to remove the placenta. You will require more intravenous drugs after the manual placenta removal for the uterus to contract (9).
- Controlled cord traction: This is performed when the placenta is separated from the uterus, but is still not able to come out. In this case, your doctor will gently pull the umbilical cord to help rid the body of the placenta (10).
- Curettage: In the case of placenta accreta, manual removal is done partially, and curettage removes the rest. Under this method, a curette is used to remove the placental debris from the uterus through scrapping (11).
Note:
Using prostaglandin E1 (misoprostol) to treat a retained placenta can be a cost-effective option. However, its safety and efficacy should be carefully evaluated by a doctor before use (11) (12).
- Hysterectomy: In the case of placenta percreta, where the placenta is deeply grown into the uterus, hysterectomy helps. It is a surgical process of uterus removal. The drawback in this treatment is you cannot carry pregnancies in the future (13).
Image: Shutterstock
Your doctor will also prescribe some oral antibiotics after any of the above treatments to prevent or treat infections.
 Did you know?
Did you know?Can You Prevent Retained Placenta?
- You cannot do much to prevent retained placenta.
- If you have experienced a retained placenta in a previous delivery, there is a higher risk of another one. You should inform your doctor so that she would pay close attention during the third stage of labor. Skin to skin contact with the baby could lessen the risk.
- Avoid prolonged use of artificial oxytocin (syntocinon) inductions so as to reduce the risk of retained placenta, caesarean section, and uterine scar. Too much oxytocin will lead to uterine atony, which is again a leading cause for retained placenta.
Frequently Asked Questions
1. What are the types of retained placenta?
There are three main types of retained placenta after a vaginal delivery. They include placenta adherens, trapped placenta, and partial accreta. These can be treated by manually removing the placenta and should be performed around 30 to 60 minutes after the delivery (14).
2. How common is retained placenta after the C section?
Retained placenta after a C section delivery is not common. It happens in three percent of vaginal deliveries (15).
3. Is retained placenta genetic?
According to a gynecology study in Sweden, the risk of retained placenta in the second generation rises if the retained placenta had happened during the mother’s birth. The risk increases if it had occurred during the father’s birth. Therefore, the study concluded an intergenerational recurrence of retained placenta on both mother’s and father’s sides (16).
4. Can retained placenta be life-threatening ?
According to a 2001 study, the retained placenta results in maternal morbidity and mortality across the developing world. It contributes to complications in two percent of all deliveries and has a case maternal mortality rate of as high as 10% in rural areas (17). A retained placenta can result in bleeding, severe infection, or even loss of life (18).
Retained placenta can cause complications and needs to be treated immediately as an obstetric emergency. Since the condition may not be preventable, it is advisable to discuss with your doctor any history of the retained placenta or any other risk factors beforehand to help with the prompt treatment. In case breastfeeding or skin-to-skin contact does not work, your doctor may proceed with other medical or surgical treatments that include removing the placenta manually, curettage or hysterectomy. Remember to stay calm amidst these and trust the process.
Infographic: Risk Factors Associated With Retained Placenta After Childbirth
Within 30 minutes of childbirth, the woman delivers the placenta in the third stage of labor. However, as presented in the infographic below, there are several reasons why the placenta may not come out easily, causing a retained placenta. Retained placenta can lead to various complications, including infection. Therefore, medical intervention is crucial in such cases.
Illustration: Momjunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Labor & delivery story | (Retained placenta).https://youtu.be/3DH3O3dNV5Y
References
- Third stage of labour.
https://www.ncbi.nlm.nih.gov/books/NBK328242/ - Shimma S Rahman et al.; (2008); Post partum haemorrhage secondary to uterine atony complicated by platelet storage pool disease and partial placenta diffusa: a case report.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2614952/ - Blake Conley Rodgers et al.; (2013); A novel treatment for management of a trapped placenta using intracervical nitroglycerin tablets.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3794125/ - Shunji Suzuki and Miwa Igarashi; (2008); Clinical significance of pregnancies with succenturiate lobes of placenta.
https://pubmed.ncbi.nlm.nih.gov/17938944/ - M H Soltan and T Khashoggi; (1997); Retained placenta and associated risk factors
https://pubmed.ncbi.nlm.nih.gov/15511838/ - C A Klufio et al.; (1995); Primary postpartum haemorrhage: causes aetiological risk factors prevention and management.
https://pubmed.ncbi.nlm.nih.gov/9599975/ - Pavol Zubor et al.; (2014); Recurrent secondary postpartum hemorrhages due to placental site vessel subinvolution and local uterine tissue coagulopathy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3943456/ - Elizabeth Abrams and Julienne Rutherford; (2011); Framing Postpartum Hemorrhage as a Consequence of Human Placental Biology: An Evolutionary and Comparative Perspective.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3168987/ - Ezinne C. Chibueze et al.; (2015); Prophylactic antibiotics for manual removal of retained placenta during vaginal birth: a systematic review of observational studies and meta-analysis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4661978/ - G Justus Hofmeyr et al.; (2015); Controlled cord traction for the third stage of labour.
https://pubmed.ncbi.nlm.nih.gov/25631379/ - Carlos F Grillo-Ardila et al.; (2014); Prostaglandins for management of retained placenta.
https://pubmed.ncbi.nlm.nih.gov/24833288/ - Treatment of retained placenta with misoprostol: a randomised controlled trial in a low-resource setting (Tanzania)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2770987/ - Clara Bodelon et al.; (2009); Factors associated with peripartum hysterectomy.
https://pubmed.ncbi.nlm.nih.gov/19546767/ - Ander D Weeks; (2008); The retained placenta.
https://pubmed.ncbi.nlm.nih.gov/1879387 - Retained placenta.
https://www.tommys.org/pregnancy-information/pregnancy-complications/retained-placenta - Margit Endler et al.; (2017); The inherited risk of retained placenta: A population based cohort study.
https://www.researchgate.net/publication/318616022_The_inherited_risk_of_retained_placenta_A_population_based_cohort_study - Retained Products of Conception.
https://my.clevelandclinic.org/health/diseases/21512-retained-products-of-conception - Ander D Weeks; (2001); The Retained Placenta.
https://www.researchgate.net/publication/318616022_The_inherited_risk_of_retained_placenta_A_population_based_cohort_study - Retained Placenta.
https://americanpregnancy.org/healthy-pregnancy/labor-and-birth/retained-placenta/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Subhashis Samajder
Read full bio of Rebecca Malachi
Read full bio of Swati Patwal
Read full bio of Dr. Joyani Das