Image: ShutterStock
Toddler staph infection is more common than in adults and is caused by staphylococcus bacteria. These bacteria can affect various body parts, including the skin and vital organs such as the lungs, and can cause serious health issues if not treated quickly. Toddlers, in particular, are at risk due to their still-developing immune systems, but adequate treatment could help prevent further complications. You may seek medical care for treating these skin lesions since OTC creams or ointments may not cure the condition. In addition, inadequate treatment could result in complications and antibiotic resistance.
Read on to know more about the risk factors, causes, symptoms, types, and management of staph infection in toddlers.
Key Pointers
- Children with malnutrition, chronic diseases, weak immune systems, exposure to unhygienic places, or contact with an infected person have an increased risk of staph infection.
- Symptoms of staph infection include skin infections, food poisoning, toxic shock syndrome, septic arthritis, pneumonia, inflammation of heart tissues, and bone infection.
- Treatments for staph infection include antibiotics (oral and intravenous), creams for minor skin injuries, and draining pus while removing infected tubes.
- Staph infection can lead to complications such as sepsis, endocarditis, pneumonia, and respiratory distress.
- Basic hygiene practices such as cleaning wounds with alcohol and properly washing utensils and food before consumption can help prevent staph infection.
Causes Of Staph Infection In Toddlers
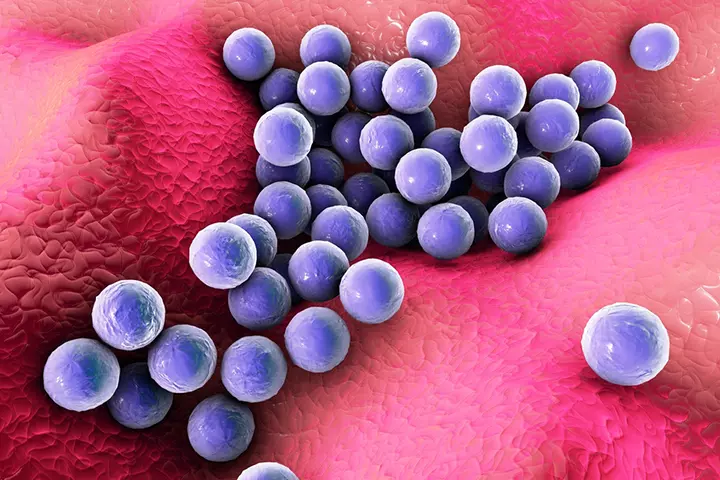
Image: Shutterstock
Staph infection can be caused by any bacteria from the genus Staphylococcus. The most common species to cause the infection is the Staphylococcus aureus bacterium. Some of the other species that cause staph infections are Staphylococcus epidermidis and Staphylococcus saprophyticus.
Staphylococcus bacteria often occur on the skin and inside the nose of healthy people, but do not cause staph infection (1). The bacteria cause infection when they enter the body through cuts, abrasions, or wounds (2). Several factors can exacerbate the risk of developing a staph infection.
Who Is At Risk Of Staph Infection?
The following factors could increase the risk of staph infection in toddlers (3) (4).
- Weak immune system or immunodeficiency
- Malnourished children
- Septic children
- Nosocomial i.e., hospital acquired infections.
- Chronic diseases, such as cancer and diabetes
- Kidney impairment that requires dialysisiA treatment that helps filter waste from the blood when a person’s kidneys fail to function properly
- Organ transplant
- HIV or AIDS
- Cystic fibrosisiA genetic disorder causing severe damage to multiple organs, including the respiratory and digestive tract
- Chronic lung disorders, such as emphysemaiA condition where the air sacs of the lungs are damaged due to prolonged exposure to air pollutants and irritants
- Skin injuries from trauma, insect bites, wounds, abrasions
- Dirty wounds
- Chronic skin disorders, such as eczemaiA skin condition that causes itchy, red, and scaly patches on the skin due to various factors such as allergies, genetics, or stress
- Hospitalization, especially for burns or surgeries
- Feeding tubes
- Breathing tubes
- Catheters and other invasive devices used during hospitalization
 Quick fact
Quick factHospital-acquired (nosocomial) staph infections are prevented by wearing gloves, gowns, sterilizing the hospital equipment, and rooms.
Eating or drinking from unhygienic places and contact with an infected person could also increase the risk of staph infection in toddlers. Toddlers who attend daycare or nurseries can be vulnerable to community-associated MRSA (Methicillin-resistant Staphylococcus aureus) from other children.
Signs And Symptoms Of Staph Infection In Toddlers
Staphylococcus may cause various types of infections ranging from minor skin infection to severe toxic shock syndrome. Signs and symptoms of staph infection may vary depending on the area affected and the severity (2) (4) (5).
1. Skin infections
Staphylococcus bacteria may cause any of the following types of skin infection.
- Boils (furuncle): It is a pus-filled pocket in the hair follicle (folliculitis) or oil gland (skin abscess) due to staph infection. Folliculitis in children can be identified by the swollen and erythematous (red) skin over the affected area. Boils are commonly seen in the underarms and on the buttocks. This superficial skin infection may drain pus if it is broken.
- Carbuncle: It is a cluster of boils usually caused by Staphylococcus aureus.
- Stye: A red bump near the eyelid due to bacterial infection.
- Impetigo (school sores): This causes large blisters or sores that ooze fluid and form honey-colored crusts. These are round, generally reddish brown. Itchy. They can spread from one part of the body to another by the child scratching. Impetigo is contagious and painful.
- Cellulitis: This involves infection of the deep skin layer, often with redness and swelling over the infected area. The whole area becomes swollen, red, hot and tender. It can occur on any body part, but generally after infected boils or impetigo. The child may develop a fever. It is extremely painful. It may open and often ooze fluids.
- Scalded skin syndrome (SSS) or Ritter disease: Toxin produced by Staphylococcus may cause the superficial skin layer to come off after a blister opens, and the skin may also appear burnt. The superficial layer of skin peels off. This condition could begin with fever and a skin rash or a blister formation.
 Quick fact
Quick factIn addition to the above, staph bacteria may also cause wound infections, such as surgical site infections or infection of burned or injured skin, when it is not kept sterile.
2. Food poisoning
Eating food contaminated with staph may cause food poisoning. Multiple institutes collaborated on a comprehensive meta-analysis to investigate the presence of Staphylococcus aureus in food, revealing a global prevalence of 30.2%. This high rate underscores the increased risk of food poisoning, with symptoms typically manifesting within a few hours of eating and lasting throughout the day.
You may notice any of the following symptoms and signs of foodborne illness in your toddler.
- Severe vomiting
- Nausea
- Diarrhea
Fever is not usually seen in staph food poisoning. It may result in dehydration and hypotension (low blood pressure) if symptoms are severe and toddlers are not hydrated well.
3. Bacteremia

Image: Shutterstock
Staphylococci may enter the bloodstream and result in bacteremia (bloodstream infection, septicemiaiThe body’s most extreme response to an infection characterized by bacteria/toxins entering the bloodstream , or blood poisoning). Fever with chills, lethargy, apathy, and hypotension are hallmark signs of blood infection. This, however, is rare and occurs in untreated bacterial infections.
Staph bacteria may travel through the bloodstream and infect internal organs, such as the heart, lung, or brain. Several body organs may be involved. This may affect muscle and bone tissue, as well.
4. Toxic shock syndrome

Image: IStock
Skin wounds and surgical wounds, when not kept sterile, may increase the risk of developing toxic shock syndrome due to staph infection. The condition can cause the following symptoms.
- High fever
- Nausea
- Vomiting
- Sunburn-like rash on palms and soles
- Diarrhea
- Reduced mental alertness or confusion
5. Septic arthritis
Staph infection of the blood may reach the joints and result in septic arthritis. It usually affects the knees, shoulders, hips, or fingers. Septic arthritis may cause:
- Fever
- Swollen joints
- Inability to move a joint due to pain
- Pus in the joints
6. Pneumonia

Image: Shutterstock
If staphylococcus bacteria reach the lung tissue, then it may lead to pneumonia. Staphylococcus aureus pneumonia is the most common cause of nosocomial pneumonia (hospital-acquired pneumonia).
Both methicillin-sensitive Staphylococcus aureus (MSSA) and methicillin-resistant Staphylococcus aureus (MRSA) strains can cause pneumonia. Antibiotic-resistant MRSA is the most common cause of ventilator-associated pneumonia (VAP) in patients who underwent ventilatory care (6).
Symptoms of pneumonia can be:
- Fever in babies and chills
- Shortness of breath
- Cough.
- Increased respiratory rate
- Indrawing of intercostal spaces
7. Endocarditis
It is the inflammation of the inner layer of the heart tissue due to bacterial infection. Flu-like symptoms are often seen in endocarditis. The symptoms of staphylococcal endocarditis can be:
- Tiredness
- Fever and chills
- Rapid heartbeat
- Swelling of arms and legs
- Breathing difficulties
8. Osteomyelitis
The infection of bone is called osteomyelitis. The following symptoms can be seen in staph bone infections.
- Fever and chills
- Redness over the affected bone
- Pain
- Swelling of the part above the bone
- Tenderness
Sometimes the bacteria can affect the central nervous system and cause central nervous system infection (CNS infection) such as meningitis. This may often occur after neurosurgeries and is not very common. Older toddlers may develop staph infection due to dental abscess. In such a case, consult a dentist promptly.
 Point to consider
Point to considerWhen To See A Doctor?
You may consult a healthcare provider if your toddler has skin infections, fever, or any other concerning symptoms. Staph infection can only be treated by a doctor who is specialized in pediatric dermatology.
A visit to the doctor is necessary if your toddler has recurrent infections with staph bacteria, and if the infection occurs along with a wound or after a medical procedure or hospitalization.
Diagnosis Of Staph Infection
A staph skin infection can be diagnosed by observing the type of skin rash or skin lesions. The following investigations are often ordered by pediatricians to confirm staph infections (7) (8) . Diagnosis is generally only clinical grounds.
- Laboratory analysis: Nasal carriage secretions or tissue samples may help identify the presence of Staphylococcus.
- Blood tests and culture: Helps identify blood infections and infection markers.
- EchocardiogramiAn ultrasound performed to assess the internal structure and functioning of the heart : Helps identify staph infections of the heart.
Depending on your baby’s signs and symptoms, the doctor may order ultrasound imaging of joints or a culture of fluid from infected joints. Sometimes CT scan or MRI is also done to detect any anomalies caused by a staph infection.
Treatment Of Staph Infection In Toddlers
Skin infections are often treated with oral antibiotics, (which is the way most staph infections are treated), while serious infections such as sepsis and septic shock may require hospitalization and intravenous antibiotics (9). Many toddlers are treated successfully in the emergency room.
Cefazolin, Zyvox (linezolid), Vibativ (telavancin), Cubicin (daptomycin) are some of the commonly given antibiotics for staph infection.
Topical antibiotic creams or antibiotic ointments can be given for minor skin injuries for infection control. You should follow the entire course of antibiotics as prescribed by the doctor even though your toddler does not show symptoms anymore.
Intravenous antibiotic treatment with vancomycin or daptomycin is often required if it is caused by methicillin-resistant Staphylococcus aureus (MRSA) strains. MRSA is an antibiotic-resistant strain of staph bacteria.
Although some skin conditions can be cured with bandages and antiseptic creams, pediatricians may recommend systemic antibiotic treatment to prevent recurrent infection.
The other treatment procedures may include:
- Pus drainage: Infected sore is incised to drain the pus and avoid complications, such as bacteremia.
- Removal of the device: If the infection is caused by medical tubes, catheters, or any other devices, then it is removed from the body.
It is not recommended to self-treat with antibiotics. Improper use of antibiotics may lead to antibiotic resistance of bacteria, thus rendering common antibiotics ineffective at treating infections.
 Caution
CautionComplications Of Staph Infections
Sepsis and bloodstream infections (BSI) are common complications of staph infections. These can affect the entire body and often lead to septic shock due to very low blood pressure. Sepsis and septic shock may lead to death if left untreated.
If staph bacteria reach endocardium (inner lining of the heart), then it could result in endocarditis (inflammation of heart lining). It may eventually lead to heart failure. This condition may result in pneumonia and respiratory distress if the bacteria reach the lungs (8).
Food poisoning due to staph bacteria could lead to dehydration and hypovolemic shockiA critical condition caused when the body loses a lot of blood or fluids, affecting the heart’s functioning if toddlers are not hydrated well on time.
Prevention Of Staph Infections
The following precautions may help reduce the incidence of staph infection (3).
- Practice good hand hygiene in the family.
- Proper hygiene.
- Proper wound care and cleaning.
- Clean all the utensils, toys, and other personal items of the baby with antiseptic solutions.

Image: Shutterstock
- Use registered disinfectants to clean the floors.
- Seek medical help for the clean dressing of an infected cut or infected skin.
- Do not share baby and toddler items with an infected family member.
- Wash food items and hands before cooking.
- Clean the vegetable cutting boards and kitchen surfaces.
You may check for adherence to hygiene precautions at daycare facilities to avoid outbreaks of community-acquired infections and MRSA infection in children. Educating caregivers and family members about recognizing the early symptoms of staph infections is also crucial.
Frequently Asked Questions
1. How long does it take for a staph infection to become serious?
The severity of staph infection may vary from one toddler to another. It usually takes four to ten days for the symptoms of staph infection to first appear and cause noticeable discomfort to the toddler (10).
2. Is rubbing alcohol good for preventing staph infections in toddlers?
Yes, rubbing alcohol is effective at preventing staph infections in toddlers. You may even rub gels containing 60% alcohol to stay protected from the infection (11).
3. Does a staph infection go away on its own in toddlers?
Yes, some cases of staph infection may heal on their own in a few weeks. However, this may vary from child to child, and it is best to consult a doctor promptly (12).
Staphylococcus bacteria causes infection when it enters the body through wounds and cuts. Toddler staph infection usually affects children with weak immune systems, malnourishment, organ transplant, and other complications. The symptoms may range from skin infections and food poisoning to toxic shock syndrome and septic arthritis. It can also cause meningitis and dental abscesses. In addition, staph bacteria are adaptable and can easily become resistant to antibiotics. Therefore, seek medical advice promptly and ensure that appropriate treatment procedure is followed. Moreover, following hygiene can help stay away from staph infections.
Infographic: Prevention Of Staph Infections In Children
Even though a staph infection in children is quite common, it is bound to be uncomfortable as it causes fever, pain, and respiratory problems, among other symptoms. So it’s better to take steps to prevent your child from going through this experience. This infographic sheds light on the preventive measures against staph infections. Read on!

Illustration: Momjunction Design Team
Illustration: Staph Infection in Toddlers: Signs Prevention & Treatments

Image: Dall·E/MomJunction Design Team
Learn how to spot the signs and symptoms of a staph infection in your child. Learn what to do if you suspect your child has a staph infection.
References
1. Staphylococcus aureus infection; The Queensland Government
2. Staphylococcal infections; Medlineplus; The United States National Library of Medicine (NLM)
3. Staph infections; healthdirect; The Government of Australia
4. Larry M. Bush ; Staphylococcal aureus infections; Merck manual
5. Staph infection; The National Health Service
6. Manisha Dahal and William R. Schwan, Management of methicillin-resistant Staphylococcus aureus mediated ventilator-associated pneumonia; The United States National Library of Medicine (NLM)
7. Diagnosing staphylococcal infections; NYU Langone Health; The NYU Langone Medical Center
8. Ana del Rio, et al., Patients at Risk of Complications of Staphylococcus aureus Bloodstream Infection; Clinical Infectious Diseases; The Infectious Diseases Society of America; Oxford Academic
9. David M. Bamberger And Sarah E. Boyd; Management of Staphylococcus aureus Infections; The American Academy of Family Physicians
10. Staphylococcal infections; Victorian Government
11. Staph infections in the hospital; Medline Plus; NIH
12. Staph Infections; Nemours Kids Health
13. Staphylococcal infections; The Royal Children’s Hospital Melbourne
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Mubina Agboatwalla
Read full bio of Dr Bisny T. Joseph
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny