
Image: Shutterstock
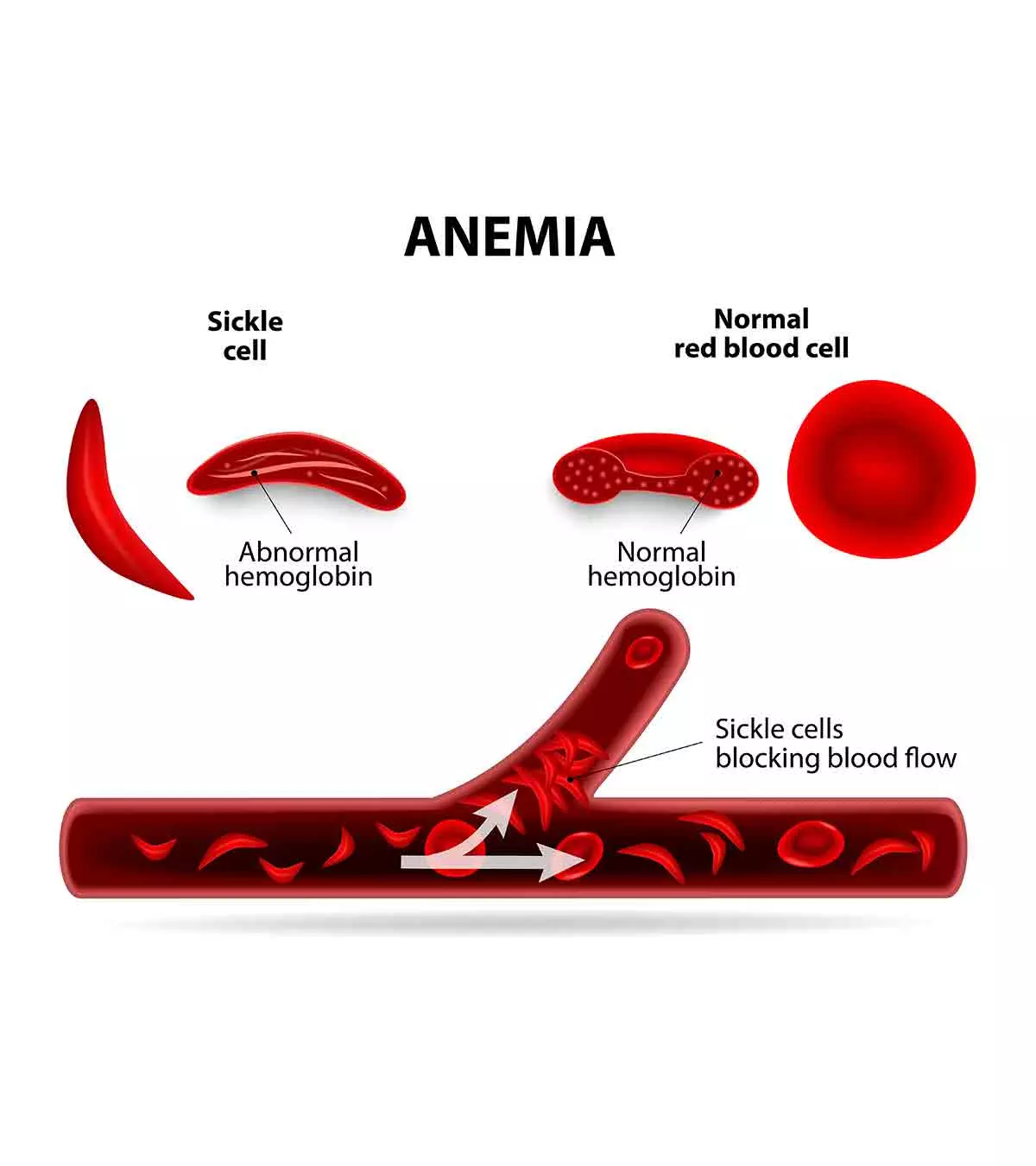
Sickle cell diseases in babies can be present from birth, and it is caused when a child inherits sickle cell genes from both parents. This inherited blood disorder makes the red blood cells (RBC or erythrocytes) crescent, sickle-shaped, or C-shaped. In addition, sickle cells can be stickier and harder than normal oval-shaped RBCs, and they may fail to move freely in the bloodstream.

The abnormal shape of the red blood cells also reduces their oxygen-carrying capacity, and tissues and organs may not get enough oxygen. This may cause pale skin, swelling on extremities, and fast breathing in most babies. Preventive measures to reduce the risk of complications could improve these issues in some cases (1).
Read on to know the risk factors, causes, signs, symptoms, complications, and ways to manage sickle cell disease (SCD) in babies.
Causes Of SCD In Babies
Sickle cell disease is a group of red blood cell disorders inherited by children from their parents. This is an autosomal recessive disease, which means that the baby will have it only if both parents are carrying the sickle cell gene (2).
- The condition occurs when a baby inherits two defective copies of the beta-globin (hemoglobin beta or HBB) gene, one from each parent. The defective copies of genes lead to the formation of a defective hemoglobin protein.
- The abnormal hemoglobin inside the RBCs forms protein chains that clump together. It distorts the shape of RBCs, causing them to become crescent-shaped or sickle-shaped, thus leading to SCD.
- The child can have both sickle cell hemoglobin (“S” gene) and normal hemoglobin gene (“A” gene) if one parent has the sickle cell gene. This situation is known as sickle cell trait and may not develop into sickle cell disease. However, the child remains a carrier of the gene and can pass it to their children.
- If parents have one child with SCD, then there is one in four chances of having another baby with the condition. There is one in two chances that the next child will become a carrier of the defective gene (3).
Types Of SCD
Types of sickle cell disease include (4) (2):
- Sickle Cell Anemia (HbSS): This is the most severe and common form of sickle cell disease accounting for 65% of pediatric cases (1). HbSS occurs due to the inheritance of two defective sickle cell genes (“S” genes), one from each parent, thus causing all hemoglobin formed in the body to be abnormal.
- Sickle Hemoglobin-C Disease (HbSC): It accounts for 25% of SCD cases among children (1). The baby receives one sickle cell gene (“S” gene) and one abnormal hemoglobin C gene (“C” gene). This form of SCD is considered mild to moderate, although symptoms may get as severe as HbSS. The onset of symptoms is often delayed to later childhood due to the presence of both normal and sickle-shaped RBCs.
- Sickle Beta Thalassemia: This is a rare form of SCD, and accounts for 10% of all cases (1). The baby inherits one sickle cell gene (“S” gene) and one defective gene for beta thalassemia. The beta thalassemia gene has two alleles (types), namely “0” and “+”. Those with the “+” gene can produce some normal hemoglobin. Therefore, HbS beta 0-thalassemia tends to be more severe than HbS beta +- thalassemia.
- Sickle Hemoglobin-D/O/E Disease (HbSD, HbSO, and HbSE ): These are forms of sickle cell disease with one inherited sickle cell gene (“S” gene) and other abnormal hemoglobin of either D, O, or E type.
Treatment and preventive measures depend on the type of sickle cell disease.
Symptoms Of SCD In Babies
Infants may not show symptoms of sickle cell disease up to four to five months of age. This is due to the presence of fetal hemoglobin (hemoglobin F) in their body during the initial months of life. The signs and symptoms eventually appear when the fetal hemoglobin is replaced by abnormal hemoglobin as the RBCs begin to sickle.
The signs and symptoms of sickle cell disease in babies may include (5) (6) (7):
- Icterus or jaundice: This is the yellowing of skin and whites of the eye due to increased levels of bilirubin produced due to breakdown or hemolysis of sickled cells.
- Anemia: This may cause your baby to become weak and irritable. Usually, red blood cells have a lifespan of 120 days, whereas sickled cells live only 10 to 20 days, thus resulting in anemia.
- Dactylitis: This is a painful swelling of fingers and toe joints. It is caused by inflammation due to blood vessels clogged by sickled cells.
- Pain crises or recurrent pain: Pain episodes are hallmark symptoms of sickle cell anemia due to blockage of blood vessels. The severity and duration of these episodes may vary in each patient.
- Frequent infections: Recurrent and frequent infections in SCD patients can be due to a non-functioning spleen as a result of spleen damage caused by sickle cell anemia.
- Vision problems: This can be due to the sickled cells clogging and damaging blood vessels in the retina of the eye.
- Delayed growth: Lack of blood cells can slow the development in infants.
The signs and symptoms of sickle cell disease will vary from person to person and can change over time.
Risks Factors For SCD
Consanguineous marriage, that is, marriage between closely related family members, is one of the most common risk factors for sickle cell disease. If there is a defective gene in the family, then there is a higher risk of it transmitting to the next generation due to a marriage between cousins. The risk can be even higher if the marriage is among first cousins (8).
People of certain ethnicities tend to have a higher risk. African, Indian, Mediterranean, Latin American, and Middle Eastern populations may have a higher risk of sickle cell disease (9).
Complications Of SCD
The signs and symptoms of sickle cell disease are related to complications of the disease. Most of these pathologies are caused by the clogging of blood vessels with sickle cells and is known as vaso-occlusive crisis. These acute crises and symptoms are called sickling crises or sickle cell crises. They may include (10):
- Acute chest syndrome is caused by blockage of the blood supply to the lungs from clogged sickle cells or a lung infection. Chest pain, fever, and shortness of breath are classic symptoms of acute chest syndrome. This is a fatal complication requiring emergency care.
- Splenic sequestration or splenic crisis is the pooling of red blood cells in the spleen, thus causing pain and enlargement. Splenic sequestration may cause damages and scars in the spleen requiring splenectomy (removal of the spleen) by the age of eight years in most children. Asplenism (lack of spleen function) can increase the risk of infection.
- Long-term anemia or chronic anemia is a lack of adequate red blood cells to carry oxygen required by the body.
- Hand-foot syndrome is caused by the lack of blood supply to hands and feet.
- The blockage of blood vessels in the brain may result in a stroke. This may cause neurological symptoms, such as reduced alertness, problems with speech, and hearing difficulty.
- Blindness or vision problems can be due to the clogging of sickled cells in the eye’s blood vessels. This may often need laser therapy to preserve vision.
- Leg ulcers or open sores are often seen in sickle cell disease.
- Extensive breakdown of red blood cells may increase the risk of gallstones due to high levels of bilirubin.
- Aplastic crisis is caused by parvovirus B19, which disrupts the precursors of red blood cells. It leads to the temporary inability of the bone marrow to create new RBCs, thus causing severe anemia.
- Multi-organ damage may happen as blood vessels get blocked due to a lack of oxygen supply.
When To See A Doctor?
Seek medical help if you notice any of the following problems (11):
- High fever
- Irritability
- Pale appearance
- Rapid breathing
- Abdominal enlargement
- Swollen feet and hands
- Weakness
- Loss of consciousness
- Vision problems
- Seizures
Diagnosis Of SCD
Diagnosis of sickle cell anemia can be made from blood tests as a part of routine newborn screening tests (2). If the infant’s blood test shows sickle cells, then your child’s doctor may request for hemoglobin electrophoresis (sickle cell test). This is useful in identifying the type of sickle cell disease and determining if the baby is only a carrier (12).
Prenatal analysis of SCD can be obtained from the amniotic fluid examinations. Identification of SCD before birth or in the newborn period could help in early management and prevention of potential complications. A detailed medical history, including family history, can also help make a possible diagnosis.
Your child’s healthcare provider may order some additional tests depending on your child’s clinical presentation to identify complications.
Is There A Cure For SCD?
Stem cell transplant
or bone marrow transplant may cure sickle cell disease. This procedure involves the transplantation of healthy bone marrow or cells from a donor to the affected person. Although it is promising, the procedures have risks and side effects, too. This is often done for severe forms of SCD to lower the complications such as organ damage (2). Sometimes finding a matching donor can be challenging, especially if the siblings are also affected.
The recent development in the treatment of sickle cell disease is gene therapy. This therapy prevents switching of fetal hemoglobin to adult hemoglobin by knocking down the expression of the BCL11A gene. This could increase the number of fetal hemoglobin, which does not lead to sickled red blood cells (13).
Treatment For SCD
The treatment may vary in each child based on the symptoms and severity of the disease. Most of the treatment options aim to improve the quality of life. Symptomatic treatments include (5) (10):
- Hydroxyurea (Siklos, Droxia, and Hydrea) helps make fetal hemoglobin and is usually given from the age of one year. This could prevent complications, delay organ damage, and may reduce the need for blood transfusion.
- Endari is an L-glutamine oral powder to reduce the pain crisis and is usually given for children older than five years.
- Voxelotor (Oxbryta) is an oral regimen to reduce anemia and SCD. It can be given to children older than 12 years.
- Crizanlizumab (Adakveo) is given to children over 16 years to reduce pain.
- Pain medications such as ibuprofen and acetaminophen (paracetamol) for fever as prescribed by a pediatrician.
- Severe anemia and other severe symptoms of organ failure require a blood transfusion.
- Antibiotics are given for secondary bacterial infection.
- Topical creams and ointments are used for leg ulcers.
Symptoms are treated depending on the clinical status, the weight of the child, and severity of the disease. Gene therapy, stem cell therapy, or bone marrow transplant may be suggested based on availability and requirement.
Prevention Of SCD
Screening of high-risk populations could help identify carriers of the sickle cell gene. Avoiding marriage between carriers could reduce the risk of SCD in children.
Although the prevention of SCD is not entirely possible, a healthy diet and good sleep could improve a baby’s general well-being.
Preventing the factors causing complications could improve the quality of life. They can be (12):
- Maintaining adequate hydration could reduce the risk of sickle cell crises due to dehydration.
- Avoiding extremely hot or cold weather and high altitudes might control triggering an acute attack.
- Following hand hygiene practices could reduce the risk of infections.
- Taking all recommended vaccines could prevent some infections.
- Getting liver and kidney function tests done, and other recommended screening tests may help detect complications sooner.
- Taking folic acid and other vitamin supplements, especially if the baby’s diet lacks folic acid-rich foods.
- Antibiotic prophylaxis involves regular antibiotic dosage from the ages of two months to five years to prevent infections. Penicillin is a common antibiotic prescribed in such cases. Research suggests that antibiotics reduce the risk of Streptococcus pneumoniae infections in children with sickle cell anemia by 84% (1).
Over-the-counter pain relievers may not be effective in managing pain and fever in a child with sickle cell disease. They may require prescription analgesics for pain management and antibiotics for infections.
Frequently Asked Questions
1. Can a child have sickle cell trait if neither parent has it?
No. It is not possible to have sickle cell trait (SCT) in a child if neither parent has the sickle cell gene. SCT only exists in a child if one parent has sickle cell trait or sickle cell disease. However, the child with SCT will be a carrier of sickle cell disease. Carriers do not develop the disease, but they can pass it to their children.
If both parents have sickle cell trait, then there is a higher chance for the child to have sickle cell disease (14).
2. Are there any vaccines that help babies with SCD?
There are certain vaccines recommended for patients with sickle cell disease to prevent some infections. They include (15):
- Pneumococcal vaccines
- Haemophilus influenzae type b (Hib) (Annual influenza vaccine or flu shot)
- Meningococcal vaccines
These vaccines could prevent certain infectious diseases that can be potentially fatal to children with sickle cell disease.
Sickle cell disease in babies is a genetic condition that reduces the body’s oxygen-carrying capacity. Infants usually show symptoms of this condition, such as jaundice, anemia, frequent urination, and delayed growth, after four to five months of age. Sometimes, they may also experience complications such as acute chest syndrome, blindness, and leg ulcers. You should contact a doctor promptly if your child experiences high fever, fast breathing, weakness, and other worrying symptoms. After diagnosis, doctors may suggest symptomatic treatment with different medications. In addition, talk to your doctor about new treatment options, such as bone marrow transplants or gene therapy.
References
- Sickle Cell Disease: Information for Parents; Healthychildren; The American Academy of Pediatrics
https://www.healthychildren.org/English/health-issues/conditions/chronic/Pages/Sickle-Cell-Disease-in-Children.aspx - What is Sickle Cell Disease?; The Centers for Disease Control and Prevention
https://www.cdc.gov/ncbddd/sicklecell/facts.html - Pediatric Sickle Cell Disease; Children’s National
https://www.childrensnational.org/visit/conditions-and-treatments/blood-marrow/sickle-cell-disease - Types of Sickle Cell Disease; Scanca Inc. – Sickle Cell Association of the National Capital Area Inc.
http://scancainc.org/learn/types-of-sickle-cell-disease/ - Sickle Cell Disease; The National Heart Lung and Blood Institute; The National Institutes of Health
https://www.nhlbi.nih.gov/health/sickle-cell-disease - Sickle cell disease; The National Health Service
https://www.nhlbi.nih.gov/health/sickle-cell-disease - Sickle cell disease; Children’s Hospital of Philadelphia
https://www.chop.edu/conditions-diseases/sickle-cell-disease-in-children-in-children - Mohammad I. El Mouzan et al.; Consanguinity and major genetic disorders in Saudi children: a community-based cross-sectional study; The United States National Library of Medicine
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6074430/ - Risk Factors for Sickle Cell Disease; Beth Israel Lahey Health; Winchester Hospital
https://winchesterhospital.org/health-library/article?id=20158 - Complications and Treatments of Sickle Cell Disease; The Centers for Disease Control and Prevention
https://www.cdc.gov/ncbddd/sicklecell/treatments.html - Sickle cell disease; Emergency Guide: When To See The Doctor; The Centers for Disease Control and Prevention
https://www.cdc.gov/ncbddd/sicklecell/documents/tipsheets_guide.pdf - ickle Cell Disease in Children; The University of Rochester Medical Center (URMC)
https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=90&ContentID=P02327 - Gene Therapy Program; Gene Therapy for Sickle Cell Disease; Boston Children’s Hospital
https://www.childrenshospital.org/centers-and-services/programs/f-_-n/gene-therapy-program/conditions-we-treat/scd - What You Should Know About Sickle Cell Trait; The Centers for Disease Control and Prevention
https://www.cdc.gov/ncbddd/sicklecell/documents/SCD%20factsheet_Sickle%20Cell%20Trait.pdf - Infections and Sickle Cell Disease; The Centers for Disease Control and Prevention
https://www.cdc.gov/ncbddd/sicklecell/healthyliving-prevent-infection.html
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Richard Mario Lurshay
Read full bio of Dr Bisny T. Joseph














