Image: Shutterstock

Tuberculosis (TB) is a chronic bacterial infection. It is a rare but contagious disease caused by Mycobacterium tuberculosis. It mainly affects the lungs but may also infect lymph nodes, bones, skin, kidneys, brain, or spine (1).
Around 1.2 million children under 15 years fall ill with TB every year (2). The Centers for Disease Control and Prevention (CDC) explains that TB in children younger than 15 years is a threat to public health as it indicates a recent transmission. As per reports by the Centers for Disease Control and Prevention, in 2025, about 4.4% of all TB cases were reported in children aged 14 years or younger. So the chance of active tuberculosis among close family members is high. Moreover, TB in young children can be life-threatening (3). Read this post to learn more about the TB symptoms, complications, diagnosis, prevention, and treatment in children.
Key Pointers
- Mycobacterium bacteria cause tuberculosis, a bacterial infection that can have adverse effects on children under fifteen years of age.
- The infection spreads when infected droplets are inhaled through the air.
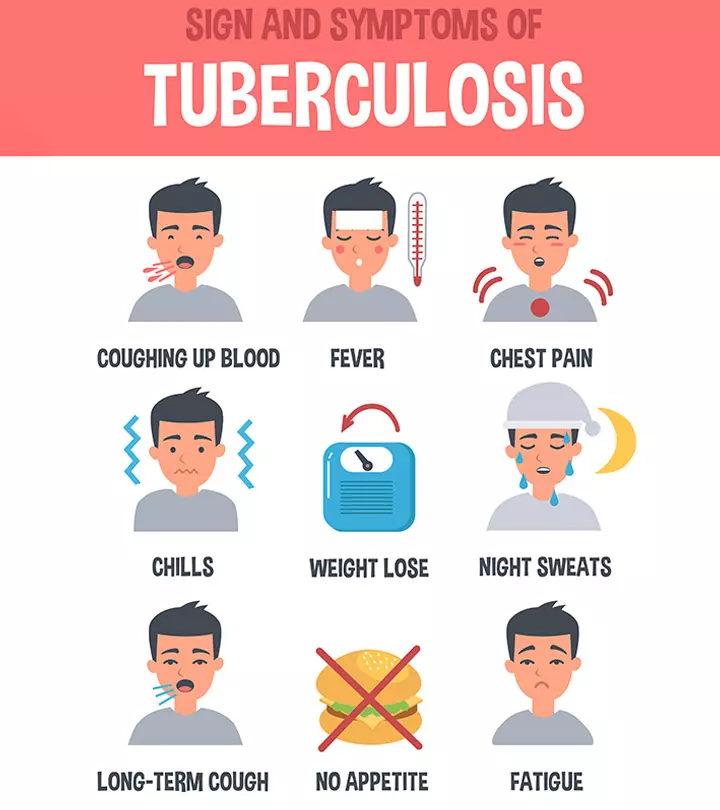
- Signs of TB in children include coughing, chest pain, blood in sputum, swollen glands, weight loss, and fever.
- Diagnosis involves conducting chest X-rays, sputum tests, CT scans, bronchoscopy, and skin tests.
- Taking the BCG vaccine can prevent TB in children.
Types Of TB In Children
The following are the different stages of TB (1).
- Exposed: This is when the child comes in contact with a TB-positive person but has a negative TB skin and blood test, a normal appearance of the lungs on an x-ray, and no correlating tuberculosis symptoms.
- Latent TB infection: This happens when the child has TB bacteria in the body but is asymptomatic. The child’s immune system causes the TB bacteria to be inactive. They test positive for TB on a blood or skin test but have a normal chest x-ray and no symptoms. They cannot spread the infection to others.
- TB disease: This is when the child exhibits the signs and symptoms of an active infection. Their blood or skin test is usually positive but may also be false-negative sometimes. Chest X-rays may be used to check for typical features of tuberculosis., but the testing shows active disease in the lungs or other sites in the body. Most children with TB are not infectious to others because of the low bacillary load.
Causes Of TB In Children

TB is caused by the bacteria Mycobacterium tuberculosis (M. tuberculosis). Most children infected with M. tuberculosis do not develop active infection and remain latent.
The bacteria is spread through the air when an infected person coughs, sneezes, speaks, sings, or laughs. A child becomes infected only on repeated contact with the bacteria. It does not spread by sharing personal items such as utensils, towels, clothing, bedding, cups, a toilet, or other items that a person with TB has touched (1).
 Point to consider
Point to considerSymptoms Of TB In Children
The TB symptoms in kids may vary according to the child’s overall health, age, site of infection, and severity of the condition. Some symptoms of tuberculosis in children include (1):
- Fever
- Night sweats
- Significant weight loss or no weight gain for a prolonged period
- Poor growth
- Cough
- Swollen glands
The following are some symptoms of TB in older children.
- Cough that lasts longer than three weeks
- Chest pain
- Blood in sputumiA thick liquid comprising mucus and saliva produced by lungs during infections

In some children, tuberculosis may spread to other organs from the primary site of infection through the bloodstream.
It may affect any vital organ in the body, and the symptoms will vary according to the site of infection.
- Brain: ConvulsionsiRapid and involuntary muscle contractions that lead to uncontrollable and rhythmic shaking of the body , lack of orientation, and loss of consciousness
- Bone and joints: Pain, swelling, and limpness
- Gastrointestinal tract: Abdominal pain and vomiting
- Water in the lungs (pleural effusion): Chest pain, heaviness in the chest, and difficulty in breathing
The treatment for such an infection needs extensive treatment (4).
 Did you know?
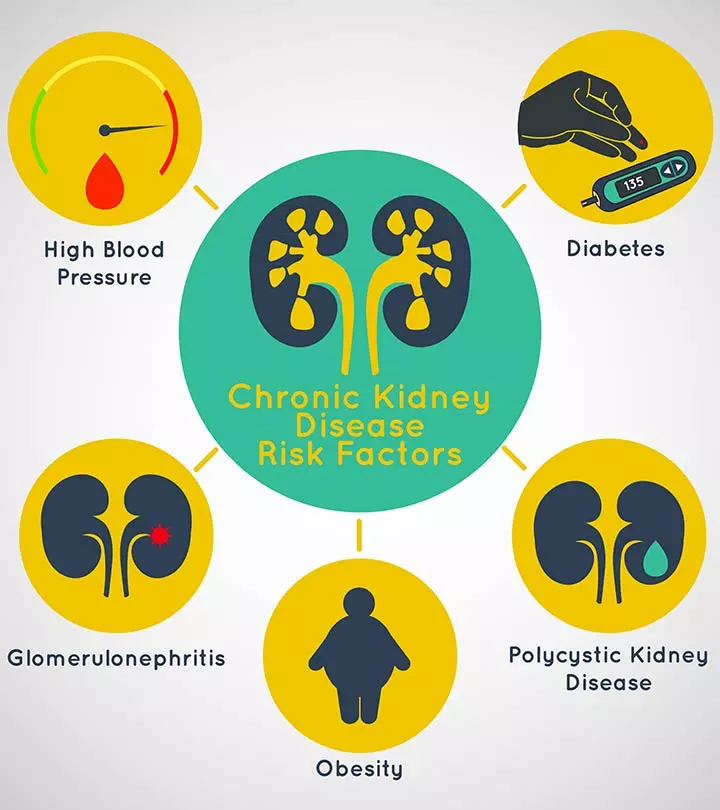
Did you know?Risk Factors And Complications Of TB In Children
The following factors may make children more susceptible to TB infection (5) (6).
- Living with or being exposed to those with TB
- Overcrowded living spaces
- Populations who are medically underserved
- Homeless and poverty-stricken population
- Living in countries where TB is prevalent
- Children living in group settings
- Children with impaired immune systems
- Unimmunized children
- Malnourished children
- Children with diabetes or HIV
- Children taking medicines such as long-term systemic corticosteroid therapyiOral or intramuscular treatment with corticosteroids, usually advised for infections and inflammatory conditions or chemotherapy as it weakens their immune system
Diagnosis Of TB In Children
The doctor will ask for a detailed medical and family history and note all symptoms of the child. They will also examine all physical signs of the child.
TB is diagnosed with a tuberculin skin test (TST). A small amount of testing material is injected into the skin, and the doctor notes the development of a bump. The size of the bump will indicate whether the test is positive or not. Local redness in the area doesn’t necessarily indicate infection.
The doctor may perform a blood test called QuantiFERON-TB Gold (QFT) or interferon-gamma release assays (IGRA), chest x-ray, sputum test, CT scan, or bronchoscopyiDiagnostic procedure that facilitates evaluation of a person’s lungs and airways with the help of a thin tube (with light and camera) for the child (7). Sputum testing is difficult in a child as children don’t expectorate sputum. So, gastric aspirateiDiagnostic procedure where ingested sputum is collected from the stomach to check for an active tuberculosis infection may be tested, but yields are very low. A TB skin test may be advised for children:
- With recent exposure to individuals with TB
- With an X-ray that looks like TB

Yearly skin tests for TB are advised for children who have HIV or live in a detention facility. Children exposed to high-risk people should be tested every two to three years.
Children may be asked to get TB skin testing from ages four to six and 11 to 16 if they:
- Have a parent from a high-risk country
- Have traveled to a high-risk area
- Live in a densely populated area (6)
Timely diagnosis of TB in children is critical for effective treatment and reducing the risk of complications. It allows for prompt treatment, reduces the risk of transmission, and improves the child’s chances of a full recovery.
Treatment For TB In Children
The treatment plan for TB is designed based on the child’s age, the site and extent of the disease, and tolerance towards specific medicines. The treatment may include (5):
- Short-term hospitalization
- Anti-tubercular drugs
- For latent TB in children, isoniazid and/or rifampicin for 3-6 months as advised by the doctor
- For active TB in children, a combination of three to four medicines, including isoniazid, rifampin, pyrazinamide, or
- streptomycin for up to six months or more, as advised by the doctor
Children usually feel better within a few weeks after the treatment starts. After two weeks of treatment, the child is no longer contagious. However, it is essential to complete the entire course of medication for maximum efficacy and to prevent relapse and drug resistance.
Prevention Of TB In Children

The main way to prevent TB in children is to take the BCG (Bacillus Calmette–Guérin) vaccine. Serious TB complications can be prevented by treating latent TB, so it does not become active. Diagnosing and treating active TB cases with the help of vaccination among adults can help prevent the spread of TB to children. Completion of the full course of treatment is absolutely essential.
If a child has TB, ask the doctor when it is safe to return to school. In addition, children in homes with active TB cases should be screened and provided preventive treatment (8).
When To Call The Doctor?
There may be some side effects from the TB medicines. Call your healthcare provider if you notice the following symptoms (7).
- Nausea
- Vomiting
- Loss of appetite
- Yellowish discoloration of the eyes or the skin
- Abdominal pain
- Tingling sensation of the toes or the fingers
- Skin rashes
- Spontaneous bleeding
- Feeling dizzy
- Tingling or numbness around the mouth
- Easy bruising
- Blurred vision
- Ringing sensation in ears
- Hearing loss
Frequently Asked Questions
1. What is multidrug-resistant TB (MDR TB)?
When TB bacteria become resistant to two or more of the most important TB medicines— INH and RIF, it is called multidrug-resistant, or MDR TB. Children with MDR TB disease need special medicines known as second-line anti-tubercular drugs. (7).
2. What happens if my child skips one dose?
If the child misses one dose, skip it and take the next dose as scheduled. Ensure your child’s healthcare provider is informed when this happens (7). The healthcare provider will add extra doses to compensate for the missed doses.
3. Why does the treatment for TB take so long?
The duration of treatment for TB is long because the TB bacteria take more time to die. It takes at least six months to clear up all the bacteria from the child’s body (7). If the infection is in the brain or bones, it will take longer.
4. How can I keep my child from spreading TB?
Completing the entire course of medicines as advised is the best way to contain TB infection. Also, encourage the child to cover their mouths with tissue paper when they cough or sneeze. Ask them to put the tissue in a closed bag and throw it away. Let your child stay at home and away from school and sleep in a separate room through the course of the illness (7).
5. Will TB cause permanent damage to my child’s lungs?
Yes, TB affects many different body systems, including the lungs. However, the extent of damage the lungs may go through depends on the severity of the disease. You should check with your doctor about this (9).
6. Which food is best for a child with TB?
Children with TB do not require any particular food. A healthy diet consisting of cereals, millets, pulses, milk, vegetables, fruits, oils, and nuts will provide enough nutrients for recovery. You can increase the energy and protein content in their meals and snacks (10).
7. How can TB treatment affect a child emotionally and psychologically?
Studies indicate that TB treatment may cause anxiety and depression in patients. However, only limited information is available in this field. More studies are required to confirm the result (11).
8. How common is tuberculosis in children?
Tuberculosis (TB) is not one of the common diseases in children. comprising about 4.4% of all TB cases in the United States in 2025. Among children aged 14 or younger, there were 364 reported cases of TB disease in that year (3).
9. What are the recommendations for treatment of latent tuberculosis infection in children?
The treatment for latent tuberculosis infection in children depends on their age and specific circumstances. Children aged two and above can take once-weekly isoniazid-rifapentine for 12 weeks. Alternatively, they may undergo four months of daily rifampin or nine months of daily isoniazid. Consulting a pediatric TB specialist before initiating treatment is recommended (12).
10. What is the role of antibiotics in TB treatment?
Antibiotic medications are vital in tuberculosis (TB) treatment. Nonetheless, TB-causing bacteria can develop resistance to these drugs, resulting in drug-resistant TB. Scientists have created spectinamides, a novel antibiotic class, to combat drug-resistant TB strains with fewer side effects. Further clinical studies are necessary to advance these medications as potential TB treatments (13).
TB is not a disease of the past. Contact your healthcare professional if your child is exposed to a TB-positive patient or exhibits symptoms similar to a TB infection. Prevention is the best way to eradicate TB. If your child is diagnosed with TB, ensure the completion of the entire course of treatment.
Infographic: Manifestations Of Tuberculosis In Organs Other Than The Lungs
Besides the lungs, tuberculosis may affect any organ in the body, but it usually affects the lymph nodes, skeletal system, gastrointestinal system, and brain. This may occur without active pulmonary infection, making diagnosis challenging, especially in children. Go through the infographic below to know some important symptoms.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Illustration: TB In Child: Types Causes Symptoms Diagnosis & Treatment

Image: Stable Diffusion/MomJunction Design Team
Delve deep into the topic of pediatric tubercilosis and learn about its causes, treatment and preventative measures from an expert.
References
- Tuberculosis (TB) in Children
https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=90&contentid=P02548 - Development of updated WHO guidelines on the management of tuberculosis in children and adolescents
https://www.who.int/news/item/07-05-2025-development-of-updated-who-guidelines-on-the-management-of-tuberculosis-in-children-and-adolescents - Tuberculosis in Children
https://www.cdc.gov/tb/about/children.html - Tuberculosis in Children and Teens
https://www.healthychildren.org/English/health-issues/conditions/chest-lungs/Pages/Tuberculosis.aspx - Tuberculosis (TB) in Children
https://www.chop.edu/conditions-diseases/tuberculosis-tb-children - Tuberculosis (TB) in Children
https://www.stanfordchildrens.org/en/topic/default?id=tuberculosis-tb-in-children-90-P02548 - Tuberculosis | Diagnosis & Treatment
https://www.childrenshospital.org/conditions-and-treatments/conditions/t/tuberculosis-tb/diagnosis-and-treatment - TB in Children – Getting, diagnosing & treating TB
https://tbfacts.org/tb-children/ - Tuberculosis (TB).
https://www.rch.org.au/kidsinfo/fact_sheets/Tuberculosis_TB/ - Food & TB.
https://tbfacts.org/food-tb/ - Habib Emami et al.; (2015); Psychological Symptoms Before and After a 14-Day Initial Inpatient Treatment in Tuberculosis Patients Compared with Their Primary Caregivers and Healthy Controls.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4745187/ - TB Treatment for Children.
https://www.cdc.gov/tb/topic/treatment/children.htm - Development of Antibiotics to Treat Tuberculosis.
https://www.nih.gov/news-events/nih-research-matters/development-antibiotics-treat-tuberculosis
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Shaon Mitra
Read full bio of Dr. Ritika Shah
Read full bio of Rebecca Malachi
Read full bio of Vidya Tadapatri