Image: Shutterstock
- Torticollis is prevalent in 16% of newborns. However, if detected early, it can be rectified even without surgery (1). So, how to identify and address the problem?
- It just takes 6 minutes to know everything about it. Read on.
- Torticollis in babies is a muscular condition in which the neck muscle of a baby becomes stiff and short.
- This condition affects the physical alignment of the baby’s head and may lead to further complications if not addressed promptly.
- Also known as infant torticollis or congenital torticollis, this muscular condition affects about 16% of the neonatal population. It causes a noticeable tilt in the infants’ heads which might be either congenital or the result of an illness. In either situation, the infant torticollis causes the neck muscle to contract, resulting in a twisted and tilted head in a bay that persists until medical attention is sought. However, if the condition is detected early enough, it can be treated without surgery (1). Learn about the causes and symptoms of torticollis in infants, how it’s diagnosed and treated, and what happens if it’s left untreated.

Key Pointers
- Torticollis affects 16% of neonates and is caused by the contraction of the sternocleidomastoid (SCM) muscle.
- The baby’s neck muscles become stiff and short, leading to a tilt in their head.
- The condition may be due to problems with fetal development, breech birth, fetal injury, or trauma during delivery.
- Acquired torticollis can occur due to an underlying health condition.
- Treatment options include physiotherapy, specialized collars, bone adjustment processes, or surgery.
What Is Torticollis?
Torticollis is the abnormal twisting of the neck due to shortening of the sternocleidomastoid (SCM) muscle
(1). SCM is a long oblique muscle originating from two points, each from the sternum (chest bone) and clavicle (collarbone). It attaches to the temporal bone – the skull bone right underneath the ears.
The SCM muscle is present on both sides of the head (2). When one muscle contracts, it pulls the neck towards its direction, while the SCM muscle on the other side expands. In torticollis, an SCM muscle contracts and remains so, thus twisting the neck towards its side. In fact, the name torticollis means “twisted neck” in Latin.
Depending on the side to which the infant’s head is turned, torticollis may be referred to as “right torticollis”, “left torticollis”, and “positional torticollis”. Despite the tautness and stiffness of the SCM muscle, torticollis is mostly painless, and infants only feel the discomfort caused by a stiff neck position.
Hope now you got a clear idea of what torticollis is. Read on to know why the problem arises in babies and what you can do about it.
What Causes Torticollis In Infants?
There are two types of torticollis viz. congenital muscular torticollis and acquired torticollis. Following are the reasons for each condition:
I. Congenital muscular torticollis causes:
Congenital torticollis, also called congenital sternomastoid torticollis, happens when the baby is born with a twisted neck or develops in the first three months of their life.
Here are the reasons for the occurrence of the condition:
- Breech birth: In breech position, the baby is born buttock first. During such a situation, the baby’s neck may get stuck in the birth canal and get stretched. It may cause the SCM muscle to tear, resulting in internal bleeding and bruising of the muscle. Over a period, the muscle develops a scar tissue that stiffens the muscle and eventually twists the neck in a direction (3).

- Developmental problems in the fetus: During the development of the fetus, its neck may twist and continue developing that way. It leads to the shortening of the SCM muscle, thus resulting in newborn torticollis. Fetal torticollis is caused by a host of reasons, but here are the most common ones viz.:
- Congenital muscular or skeletal abnormalities. For example, Klippel-Feil Syndrome, where bones of the neck fuse together thus causing a tilt in the head (4).
- Intrauterine problems. Excessive uterine tissue may cause the fetus to cramp thus leading to the shortening of the SCM muscle.
- Fetal injury. The physical impact to the womb may alter and affect the development of the fetus. It may cause defective shortening of the neck muscle, and the baby would be born with a head tilt.
Note:
Sometimes, skull deformities, such as brachycephaly (wide, shortened head shape) and craniosynostosis (abnormal head shape due to skull bones fusing too early) may cause torticollis. However, most cases of infant torticollis are not related to skull deformities.
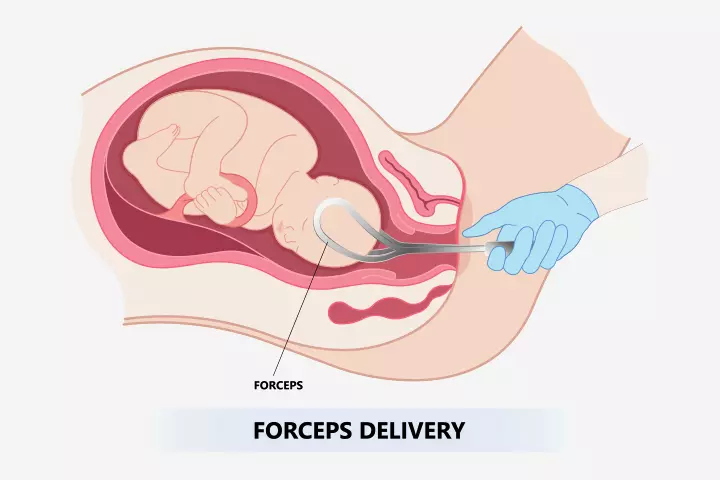
- Traumatic delivery: A baby stuck in the birth canal during normal delivery would have to be brought out using forceps or suction. The tremendous force of extraction during a difficult birth can cause SCM muscle trauma. An improper use of ancillary delivery equipment can also lead to tissue damage and subsequently torticollis.
II. Reasons for acquired torticollis in babies:
Acquired torticollis occurs as a side-effect of a health condition and is not seen at the birth of the infant. Below are the causes for acquired torticollis:
- Ocular torticollis: Babies with eye misalignment may have trouble perceiving depth and distance. To compensate for the flawed vision, the infant tilts their head to see properly. A baby with extended tilted positioning will shorten the developing SCM muscle, eventually leading to ocular torticollis (5). The condition is also called ocular abnormal head posture.
Ocular torticollis is considered a non-musculoskeletal reason for torticollis since the baby would have been born with a healthy SCM muscle (6). Even the torticollis could be mild. However, the problem lies in the ocular muscles, which are responsible for the movement of the eyeballs.
- Sandifer’s syndrome: Babies suffering from severe gastroesophageal reflux disease (GERD) may develop a rare pediatric disorder called Sandifer’s syndrome. In this condition, a baby has an abnormal contraction of the muscles along with bouts of reflux. It causes the infant to make awkward body movements called dystonia, which includes head-tilting and holding the neck in a torticollis-like position (7). It is triggered by SCM muscle spasms induced by nerve impulses. Acquired torticollis due to reflux is extremely rare (8).
- Benign paroxysmal torticollis: The infant tilts the head regularly for long periods, from a few hours to days. The tilt happens in any random direction, and the baby will go back to normal after an episode of torticollis. Recurrence is common, and the condition is accompanied by other symptoms like disorientation, drowsiness, and irritability (9). The problem peaks during the first 12 months of a baby’s life and usually disappears after the age of five (10). The causes for benign paroxysmal torticollis are not known, but it is believed to be caused by problems in the nervous system rather than the muscles. The disorder has been linked to a genetic mutation that plays a role in other neurological problems like a migraine and vertigo.
- Grisel’s syndrome: An infection in the nasopharyngeal channel may cause inflammation of the neck muscles, which results in subluxation (dislocation) of the atlanto-axial joint. The joint lies between atlas and axis – the first two cervical vertebrae in the neck. Dislocation can happen even due to an infection in tonsilsiTonsils are oval-shaped tissue masses located at the back of the throat and help fight infections. , adenoidsiThe adenoid is a mass of tissue behind the nasal cavity. , and middle ear. The syndrome has also been reported after surgical procedures like a tonsillectomyiThe surgical removal of the tonsils. or adenoidectomyiThe surgical removal of the adenoids, primarily performed on children. (11). The dislocated joints permanently bend in one direction leading to the classic head tilt of torticollis. Ear, nose, throat (ENT) infections are considered the primary cause of the problem. Grisel’s syndrome can happen at any age but is most common in juveniles (12).
- Neural axis abnormalities: The deformities of the spine can cause a change in the axis that is the alignment of the spinal cord. A change in the alignment disturbs the motor nerves, making them twitch the muscles. A contraction of the SCM muscle eventually leads to torticollis. Skeletal disorders like scoliosisiA condition where the spine curves to the side, often in an S or C shape. are often the reason behind neural axis abnormalities (13).
- Spasmus nutans: This condition displays three problems simultaneously – head nodding, torticollis, and nystagmus, which is the rapid involuntary movement of the eyes. The causes of spasmus nutans are unknown, but the condition is linked to a deficiency of iron and vitamin D, and brain disorders (14). Many experts believe the problem to be ophthalmic since vision is impacted due to quick eye movement. The patient compensates for it by nodding and tilting of the head (15).
- Infection and injuries: Babies can be affected by torticollis even for general reasons such as a direct injury/trauma to the neck. Infections to the cervical spine and its surrounding tissue can also eventually cause a tilt of the head (16).
 Things to know
Things to knowA twisted neck is the primary symptom of torticollis, but there are other signs to identify the condition.
Next we tell you about the various other signs to identify torticollis.
What Are The Symptoms Of Torticollis In Babies?
Tilted neck is the classic symptom of torticollis. Nevertheless, parents can look for the following signs of probable torticollis:
- Infant turns head only one way. For instance, if the baby suffers from right torticollis (head tilted towards the right), then he will always move the head to the left. If the baby has to look to the right, then he moves his entire body to the right.
- The infant prefers one breast for feeding. Since torticollis causes a limited range of head motion, the baby may have trouble latching to a breast. He may not act fussy while feeding on the other breast but will seem comfortable and contented when feeding on one.
- There is a thick lump of muscle on the neck. The presence of a lump indicates scar tissue. If the baby had an SCM muscle injury, then the parent can spot a small pea-sized lump on the muscle.
 Quick fact
Quick factYou can look out for these symptoms, which are clearly visible. If the signs are indicating torticollis, you need to go for a professional diagnosis to ensure that the baby is treated promptly.
Sometimes, a child with benign paroxysmal torticollis (BPT) may have additional signs and symptoms during the attacks. The graph below shares those symptoms and their prevalence.
According to the data, ataxia (79%) and irritability (79%) are the most commonly associated symptoms during BPT episodes, followed by vomiting (77%) and pallor (66%). Additional associated symptoms include photophobia, poor oral intake, motion sensitivity, abnormal trunk posture, phonophobia, and limb dystonia.

Symptoms associated with Benign Paroxysmal Torticollis (BPT) episodes
Source: Benign paroxysmal torticollis: phenotype, natural history, and quality of life; Pediatric ResearchHow Is Torticollis Diagnosed?
The healthcare professional will use one of these three ways to diagnose torticollis in babies:
- Visual and physical inspection: The obvious way to determine torticollis is through the inspection of the infant. The doctor may move the baby’s head and feel for any resistance from the SCM muscle. If the baby’s neck muscle was injured during delivery, then the physician will look for any external signs of scar tissue. Inspecting the baby right after the birth and again after a few days can help detect torticollis early. In the case of acquired torticollis, doctors look for the symptoms of any other health condition and will ask you about the infant’s medical history.
- X-ray: An X-ray gives a clear picture of the underlying bone structure. It helps detect the presence of torticollis or any other skeletal disorder in the baby.
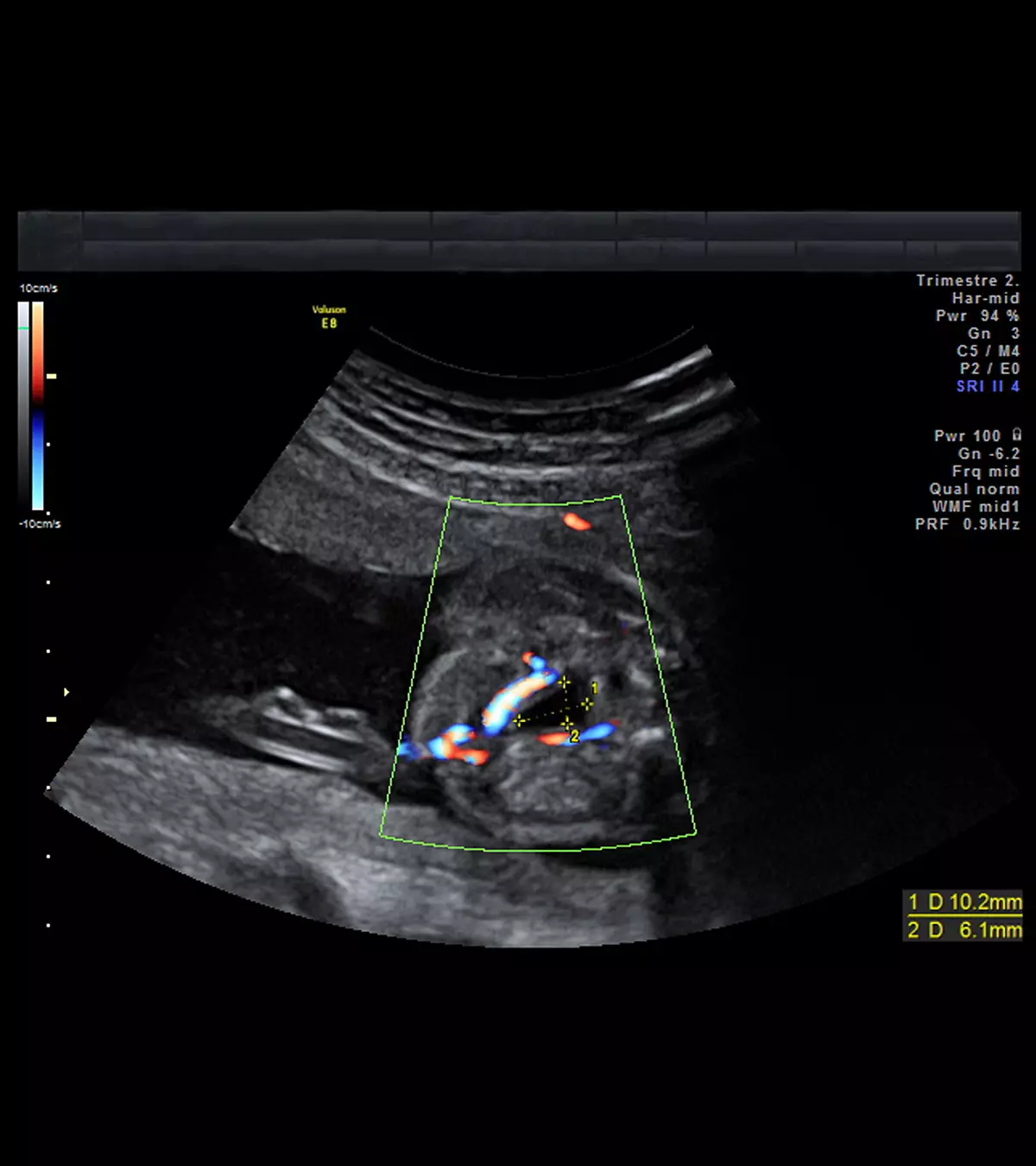
- Ultrasound analysis: Ultrasound imaging is done with high-frequency sound waves, which establishes an accurate image of muscles and blood vessels. By assessing an ultrasound picture, the doctor can tell for sure whether the SCM muscles suffer from a problem.
The treatment for torticollis need not always be surgical. Coming up is a list of treatment options for the problem.
Once the doctor confirms that it is torticollis, they will initiate the treatment right away.
How Is Torticollis Treated?
If the torticollis is acquired as a side effect of another disorder, then the doctor will treat that particular condition. If torticollis is a problem in itself, it could be treated in one of the below methods:
- Physiotherapy is a non-invasive way of treating torticollis. Neck stretches, massages, and exercises can be done at home either by the parent or by a professional. If the parent has to take up the responsibility, they need to be trained by a certified pediatric physiotherapist. Stretches will be accompanied by scheduled visits to the pediatrician and physiotherapist to assess the progress of the treatment.

Remember, a parent must never attempt head stretch and neck movement on the baby without medical guidance and training. Consultation with a medical professional is necessary before performing any move on the baby’s delicate neck.
Stretches help release the tension in the SCM muscle and expand it back to its normal shape. The baby’s head is stretched gently in various directions thus reducing head tilt. An exercise regime ensures complete recovery of the muscle with its full range of motion.
- A specialized infant tubular orthosis for torticollis (TOT) collar is a simple plastic frame that can be secured on a baby’s neck (16). It is also referred to as a brace.

The TOT collar straightens the neck by putting gentle pressure on the opposite side of the tilt. It slowly brings the neck to the correct alignment by stretching the SCM muscle. The orthopedic doctor will train the parents in putting on and taking off the collar. The baby will have to wear the collar for a prescribed number of hours every day. Most collars are washable since they are made from plastic or washable fabric. TOT collars are most likely to be recommended in combination with physical therapy.
- A chit is a type of treatment that focuses on bone adjustment to relieve tension on muscles and nerves. The alternative medicine works well with other forms of non-invasive treatments such as physiotherapy. In a chiropractic adjustment, the chiropractor (a doctor) uses his hands to adjust the baby’s spine with calculated and precise moves. It is not a standard bone setting as the practitioner will conduct a detailed assessment before doing the adjustment. Chiropractic adjustments have been found to be effective at curing neck tilt, and experts believe it should be considered an option for torticollis treatment in infants (17).

- Botox: Botulinum injections, also known as Botox, can help relieve the tautness of SCM muscle and reduce the head tilt. Botox injections are formulated using botulinum toxin secreted by the bacteria called Clostridium botulinum. The dose is directly administered to the SCM muscle to release its tension. An infant may have to undergo more than one injection depending on the intensity of torticollis.
Botox is considered a midway between physical therapy and surgery since it is suitable for infants, who do not respond to physiotherapy but the condition is not severe enough for surgery. Botox is used for the treatment of spasmodic torticollis in adults, and researchers find botulinum injections effective even for babies with torticollis (18). However, the treatment is ideal for infants above six months of age.
- Surgery: It is the last option if the baby does not respond to any other interventions. The surgery for torticollis in infants aims to reduce the SCM muscle tension and achieve a complete neck extension without any tilt. The exact surgical process depends on the severity of the torticollis. A standard operating procedure involves making an incision at the lower attachment point of SCM muscle on the chest. Here, the muscle is stripped from the bone, allowed to relax, and reattached with the corrected neck position (19).
Surgical procedures are followed by intensive physiotherapy sessions that help reinforce the stretchiness of the muscle. The infant will also have to wear a brace to maintain the correct position of the head. Once the muscle heals and sets into place, the infant can be free of torticollis.
Recovery Time
The treatment works best when initiated before the age of six months when the baby has a flexible musculoskeletal system. Whereas physical exercises can take six months or more to show positive results, surgical intervention shows immediate results, but in the latter case, the baby will have to undergo physical therapy for more than three months to reinforce the muscle’s position. In either case, it can take months before the infant holds his head straight. It is worth the wait because if left untreated, torticollis can lead to other complications.
Torticollis may not seem to be a serious ailment but if left untreated, it can lead to some long-term problems. Read on to know what they are.
Long Term Effects Of Torticollis
If the baby suffers sustained torticollis then the following collateral problems may emerge:
- Plagiocephaly: Torticollis may cause positional plagiocephaly, also known as flat head syndrome, where an infant’s head flattens because of repeated sleeping on one side due to neck tilt (20). The condition needs to be managed along with torticollis. For plagiocephaly, a baby will have to undergo a helmet therapy where a helmet-shaped head brace gently squeezes the skull bone back to shape (21).
- Facial asymmetry: Facial asymmetry happens when one side of a face is excessively dissimilar to the other side. Since the infant will tend to tilt the head in one direction, the facial muscles and attributes slowly align the wrong way. Asymmetry can happen with any type of torticollis but is most common in ocular torticollis. Correction of torticollis helps improve the condition.
- Skeletal disorders: Infants suffering from torticollis have a significantly higher risk of developing other skeletal problems (22). A baby with torticollis will tend to align other parts of the body the wrong way to counterbalance the effects of tilted head. The voluntary skeletal misalignment causes bones to fuse incorrectly thus leading to skeletal complications like hip dysplasia (hip dislocation), metatarsus adductus (deformed foot), and talipes equinovarus (bent foot).
Timely initiation of torticollis treatment is all you need to do to prevent the above conditions. Parents can always play a part in helping the baby come out of the problem.
Ashley Riley, who has a son with torticollis, shares her own story to show how important it is to find and treat the problem early. Even though Ashley and her husband suspected something was wrong with their son’s spine, the doctors who checked him until he was 15 months old told her that everything was okay.
She recalls, “It was only during our son’s 15-month checkup when we met an attending physician who instantly recognized that something was wrong. He noticed how our son’s entire upper body seemed bent to the left while the torticollis in his neck, despite our efforts to address it, curved to the right. On that very day, he ordered an MRI to be performed.” The MRI results revealed a severely twisted spine, a condition that could be life-threatening if not treated properly. Vital organs, including the heart and lungs, were at risk, and it might require multiple surgeries.
She continues, “It wasn’t until three pediatric orthopedic consultations later that we would finally get the full picture of his prognosis. His spine was not only curved, it was rotated inward. He was missing ribs. Two of his neck vertebrae were fused together (i).”
How Can Parents Help A Baby With Torticollis?
There are some baby-safe means to counteract the effects of torticollis right at home. Here is what you can do:
- More tummy time: Pediatric experts vouch for all the positive effects this simple activity has on the baby’s overall physical development. Tummy time strengthens the baby’s neck and back muscles. It stimulates the baby to use multiple muscles.
- Baby, look the other way! One way to rectify the baby’s neck tilt is to encourage them to turn in the opposite direction. Use food or toys to lure the infant to turn in order to stimulate the natural and voluntary extension of the neck muscle. During feeds, the mother can place the bottle or feed the baby on the breast in the opposite direction of torticollis. Such stimulation relaxes and conditions the SCM muscle thus providing relief from torticollis in the long run (23).
 Quick tip
Quick tip- Watch the sleeping position: Parents must avoid carriers that immobilize the baby in one single position since it can increase the risk of plagiocephaly/flat head. Parents can use a torticollis pillow to support the baby’s neck while sleeping. Experts recommend the use of specialized pillows to help babies sleep better (24). However, take your doctor’s advice before using a pillow.
The process of curing torticollis is slow and long. You need to deal with it carefully so that the muscles of the baby are not damaged.
Now you know that torticollis is treatable but is it preventable?
Can We Prevent Torticollis?
There is no way to prevent congenital torticollis caused by genetic mutations. However, there are a couple of things parents can do to reduce the risk of torticollis in babies:
- Have a safe delivery: As mentioned above, a breech baby has a risk of developing torticollis due to a neck injury while birthing (birth injury). If the doctor feels that a breech natural delivery could harm the newborn, then a C-section could be performed. This is highly situational and a doctor may decide it considering several factors at that moment. Nevertheless, strive for the safest mode of birth to minimize the risk of torticollis in the newborn.
- Look for early signs of torticollis and torticollis-related problems: Acquired torticollis could be the result of some health condition, including other skeletal disorders. Be watchful for the signs as early diagnosis ensures a higher success rate of treatment.
Frequently Asked Questions
1. Does torticollis cause developmental delays?
Studies have shown that infants with torticollis may have a slow gross motor (GM) development without any effect on their cognitive development. However, the delay in GM development can normalize in a year (25).
2. Can baby torticollis resolve itself?
Torticollis may self-correct, provided it is treated within a month or two of the onset. A delay of more than three months might also delay the treatment (26).
3. Can torticollis in babies affect their speech or other developmental milestones?
The signs of torticollis in babies are evident. Hence, a medical professional can make an initial diagnosis on observation. However, they may suggest an ultrasound or an X-ray to confirm their speculation. The treatment would be dependent on the cause, and it may be treated non-surgically if detected in the early stages. Despite the form of the treatment, the recovery time for torticollis in babies may take months based on the intervention. Keep an eye on your baby’s head position and encourage tummy time to strengthen their neck muscles and assist them in their recovery.
Infographic: Possible Causes Of Torticollis In Babies
Babies can either have torticollis at birth, or they might develop or acquire the condition during infancy. Therefore, knowing the causes can help in early diagnosis, intervention, and correction of this condition in babies. The following infographic enlists possible causes of torticollis in babies.
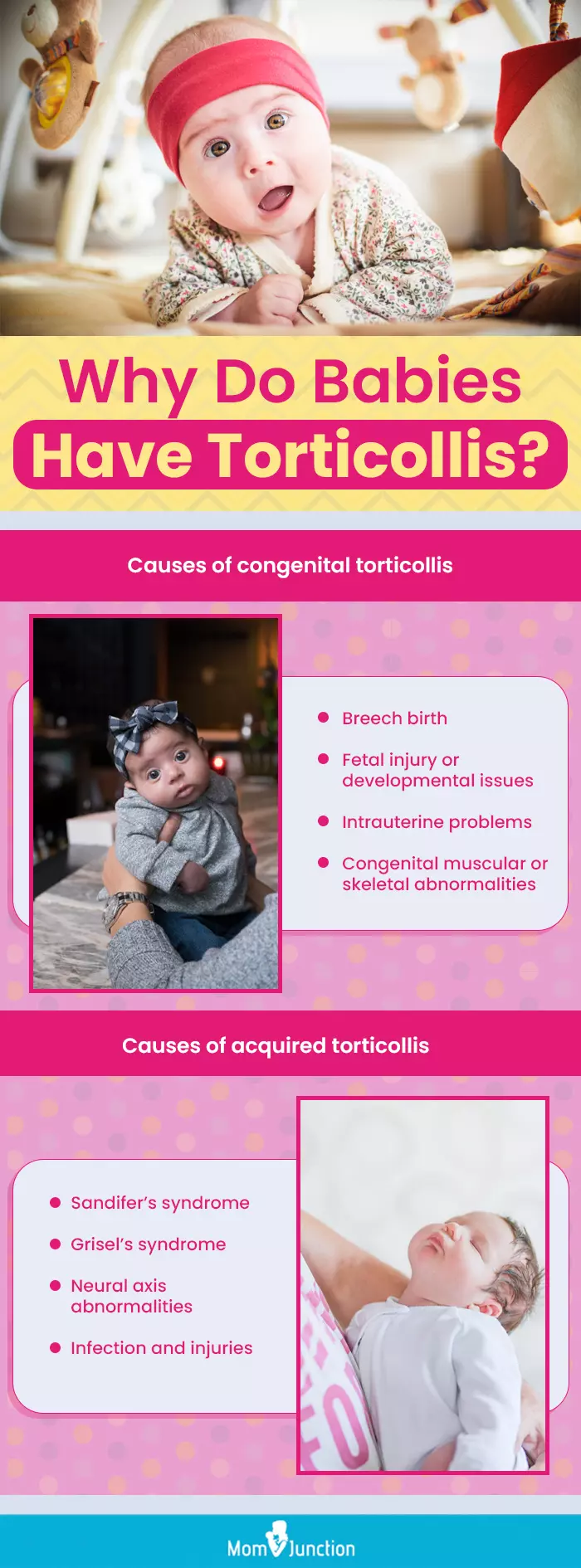
Illustration: Momjunction Design Team
Illustration: What Is Torticollis In Babies Its Signs And Treatment

Image: Stable Diffusion/MomJunction Design Team
Torticollis is a condition where the neck muscles become tight, causing the head to tilt to one side. Learn more in this video!
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. I worked for a hospital that misdiagnosed my son’s chronic condition.https://medium.com/modern-parent/i-worked-for-a-hospital-that-misdiagnosed-my-sons-chronic-illness-338fec77da47
References
- Congenital Muscular Torticollis and Positional Plagiocephaly.
https://publications.aap.org/pediatricsinreview/article-abstract/35/2/79/32479/Congenital-Muscular-Torticollis-and-Positional?redirectedFrom=fulltext - Bruno Bordoni and Matthew Varacallo; Anatomy, Head and Neck, Sternocleidomastoid Muscle.
https://www.ncbi.nlm.nih.gov/books/NBK532881/ - Congenital Muscular Torticollis.
https://www.stanfordchildrens.org/en/topic/default?id=congenital-muscular-torticollis-90-P02070 - Head Tilt (Torticollis).
https://www.healthychildren.org/English/health-issues/conditions/Cleft-Craniofacial/Pages/Head-Tilt.aspx - Mohammad Reza Akbari et al.; (2015); Facial asymmetry in ocular torticollis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4877722/ - S E Rubin and R S Wagner; (1986); Ocular torticollis.
https://pubmed.ncbi.nlm.nih.gov/3523807/ - Burcin Nalbantoglu et al.; (2013); Sandifer’s Syndrome: a Misdiagnosed and Mysterious Disorder.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4025139/ - Martin J Herman; (2006); Torticollis in infants and children: common and unusual causes.
https://pubmed.ncbi.nlm.nih.gov/16958498/ - Adamos Hadjipanayis et al.; (2015); Benign paroxysmal torticollis of infancy: An underdiagnosed condition.
https://pubmed.ncbi.nlm.nih.gov/25644090/ - N J Giffin et al.; (2002); Benign paroxysmal torticollis of infancy: four new cases and linkage to CACNA1A mutation.
https://pubmed.ncbi.nlm.nih.gov/12162387/ - C Bocciolini et al.; (2005); Grisel’s syndrome: a rare complication following adenoidectomy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2639892/ - Davide Allegrini et al.; (2016); Grisel’s syndrome, a rare cause of anomalous head posture in children: a case report.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4774015/ - Jun Qiao et al.; (2013); Indication for preoperative MRI of neural axis abnormalities in patients with presumed thoracolumbar/lumbar idiopathic scoliosis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3555633/ - Spasmus nutans.
https://medlineplus.gov/ency/article/001409.htm - Spasmus Nutans.
https://eyewiki.org/Spasmus_Nutans - Torticollis.
https://www.childrenshospital.org/conditions/torticollis#:~:text=Congenital%20muscular%20torticollis - Mette Hobaek Siegenthaler; Chiropractic Management of Infantile Torticollis With Associated Abnormal Fixation of One Eye: A Case Report.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4371108/ - Botulinum Toxin Type A in the Treatment of Children with Congenital Muscular Torticollis.
http://regispthomeexerciseprograms.pbworks.com/f/botox+for+torticollis.pdf - Kumar Nilesh and Srijon Mukherji; Congenital muscular torticollis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3814673/ - Torticollis and plagiocephaly in infancy: Therapeutic strategies.
http://regispthomeexerciseprograms.pbworks.com/f/torticollis%20tx-systematic%20review.pdf - Baby Helmet Therapy: Parent FAQ.
https://www.healthychildren.org/English/health-issues/conditions/Cleft-Craniofacial/Pages/Baby-Helmet-Therapy-Parent-FAQs.aspx - Torticollis.
https://pedclerk.uchicago.edu/ - Heads Up: 5 Tips to Help Your Baby Who has Congenital Muscular Torticollis at Home.
https://www.hss.edu/condition-list_congenital-muscular-torticollis.asp - Plagiocephaly (Flat Head Syndrome).
https://my.clevelandclinic.org/health/diseases/10691-plagiocephaly-flat-head-syndrome - Motor and cognitive development at one-year follow-up in infants with torticollis.
https://www.researchgate.net/publication/6444403_Motor_and_cognitive_development_at_one-year_follow-up_in_infants_with_torticollis - What You Can Do to Help Relieve Your Baby’s Torticollis.
https://health.clevelandclinic.org/torticollis-how-parents-can-help-correct-a-babys-head-tilt - Motor Speech Disorders and Congenital Muscular Torticollis: A Case Series.
https://www.eacademy.hss.edu/courses/motor-speech-disorders-and-congenital-muscular-torticollis-a-case-series - Motor ASpeech Disorders.
https://www.stonybrookmedicine.edu/patientcare/speechhearing/speechlanguage/motordisorders#:~:text=Motor%20Speech%20disorders%20are%20characterized
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Vineet Kwatra
Read full bio of Rohit Garoo
Read full bio of Dr. Ritika Shah
Read full bio of Shinta Liz Sunny