Image: Shutterstock
The umbilical cord is a three-vessel cord (having two arteries and one vein) that connects the fetus to the placenta. However, the umbilical cord undergoes irregularity in some women and becomes a two-vessel cord (having one artery and one vein). The exact cause of the formation of a two-vessel cord is unknown, but a few theories try to explain the condition. The presence of this umbilical cord may lead to certain complications, so doctors monitor such pregnancies closely to ensure the baby grows properly. Read the post to get more information on a two-vessel cord, its causes, associated pregnancy risk factors, and effects on the baby.
Key Pointers
- The umbilical cord happens to be formed during the fifth week of pregnancy and provides critical nutrients and oxygen to the fetus.
- A two-vessel cord is an abnormal condition in which the umbilical cord has one vein and one artery, instead of two.
- Risk factors for a two-vessel cord include maternal age (above 40), smoking, diabetes, or high blood sugar.
- The condition may sometimes increase the risk of preterm birth or fetal abnormalities.
- To avoid any complications associated with the two-vessel cord, timely medical checkup is recommended to see the baby’s growth.
What Is A Normal Umbilical Cord?
The formation of an umbilical cord begins during the fifth week. It connects the fetus to the placenta during pregnancy. It measures around 20in (50cm) in length.
Normally, an umbilical cord has two arteries and one vein. It is also known as a three-vessel cord, which is covered by a thick gelatinous substance called Wharton’s jelly (8).
Here’s what the blood vessels in the umbilical cord do (8):
- The vein carries nutrients and oxygen from the mother to the fetus.
- The arteries carry the waste products like carbon dioxide and deoxygenated blood away from the fetus to the mother’s bloodstream, to eliminate them through the mother’s kidneys.
In some cases, obstetric complications arise due to a change in the number of blood vessels in the cord. One such abnormality is a two-vessel cord.
What Is A Two-Vessel Cord?

In a two-vessel cord, there is one vein and just one artery instead of two. It is also called single umbilical artery or SUA. It may affect 0.5–6% of all pregnancies worldwide with a higher incidence in twin pregnancies (1). Research shows SUA affects about 1 in 100 singleton pregnancies and about 5 in 100 multiple pregnancies. Additionally, every 2 in 10 babies with SUA may have a health condition associated with the kidney, heart, or digestive system, or they may have a genetic condition (9).
 Quick fact
Quick factWhat Causes This Umbilical Cord Abnormality?
Though the precise cause of the two-vessel cord is unknown, there are three theories around it.
As per one theory, this condition arises because one of the two arteries stops growing inside the womb, while another theory suggests improper splitting of the artery into two (2). A third theory states that SUA may result due to the persistence of the original allantoic artery of the body stalk present in the human embryo (10).
As mentioned earlier, this condition occurs in less than 1% of singleton pregnancies, but some women are at a higher risk than others.
What Are The Risk Factors For A Two-Vessel Cord?

Here are the factors that could make a woman susceptible (11) (4):
- Pregnancy after 40 years of age
- Multiple pregnancies
- Smoking
- MultiparityiRefers to a woman who has given birth more than once
- Pregnant with a girl
- History of diabetes or episodes of high blood sugar
- Occurrence of Velamentous cord insertioniA pregnancy complication where the umbilical cord inserts into the fetal membranes (amnion and chorion) instead of directly into the placenta (VCI)
Ethnicity (such as being a Caucasian woman) and having a maternal history of seizure disorders are some other risk factors that may contribute to a slightly higher incidence of SUA. However, this condition can also arise without any risk factors threatening neonatal health. In most cases, the baby is normal, but in a few cases, there could be problems associated with fetal development and SUA.
How Is A Two-Vessel Cord Diagnosed?
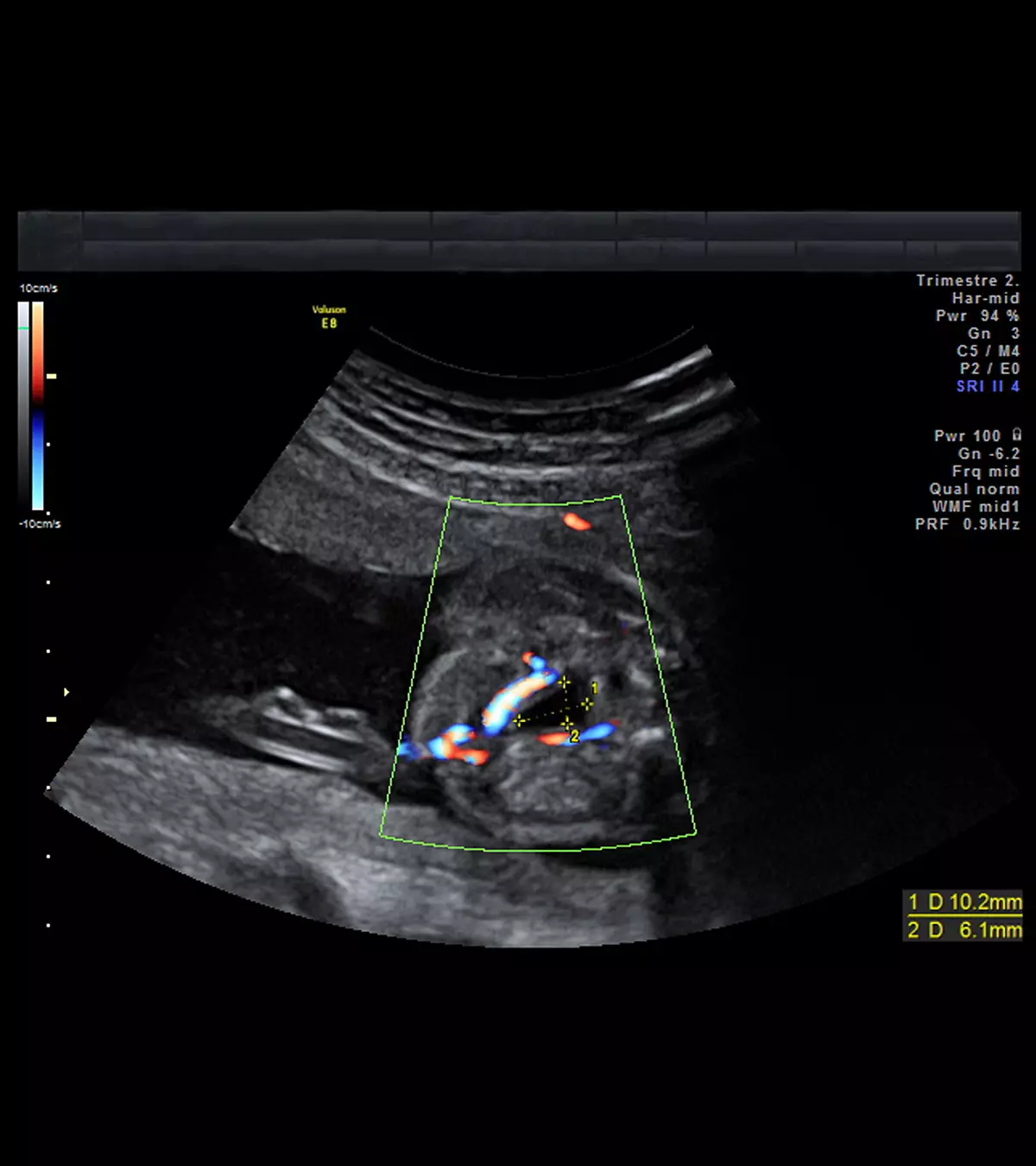
The SUA can be detected during a prenatal ultrasound scan. Usually, the doctors check for the umbilical arteries during the 18th week of gestation. A color-flow Doppler ultrasound can help detect this abnormality earlier. It is usually done in the 14th week. A high-definition Doppler ultrasound scanner can further help to determine which side of the umbilical artery is missing (12).
The doctors also assess the problem by checking (9)(10):
- Your family and personal medical history
- Detailed fetal ultrasound

- Fetal echocardiogram to check the functioning of the fetal heart
- Genetic abnormality screening such as an aneuploidy screening
- Amniocentesis at 15 to 20-week obstetric visit to detect birth defects and genetic conditions
One or more of these tests will help with a prenatal diagnosis and help you know if it is going to affect the baby. Also, your doctor will suggest regular monitoring of your baby through ultrasounds to ensure proper fetal growth and detect any abnormalities as soon as possible.
 Did you know?
Did you know?Does Single Umbilical Artery Pose A Risk To The Baby?
SUA need not necessarily harm your baby. Sometimes, it doesn’t result in pregnancy complications (3). However, in some cases, there is an increased risk of birth defects, which include (4):
- Intrauterine growth restrictioniA condition when the fetus is smaller than what is expected for their gestational age leading to fetal malformations (requires serial follow-up)
- Congenital heart problems
- Kidney problems (postnatal urinary infection)
- Restricted growth of the central nervous system
- Preterm labor and premature birth
- Gastrointestinal problems
- Edwards syndromeiA chromosomal condition caused by an extra copy of chromosome 18 (Trisomy 18)
If the doctor finds no adverse effects of the two-vessel cord on the baby, then it is called an isolated single umbilical artery. In such a case, another ultrasound screening is recommended in the later weeks for fetal monitoring to see if the baby is growing in proportion to their gestational age.
If the obstetric ultrasound findings indicate any probable abnormalities regarding the pregnancy outcome, the doctor suggests an amniocentesis (a sample of amniotic fluid is tested after ten weeks for congenital abnormalities in the fetus). If the baby is born with organ dysfunction, then extra care is provided in the NICU.
A mom and blogger who goes by the name “Pioneer Mom” shares about her second pregnancy when she was diagnosed with the two-vessel umbilical cord. She says, “While pregnant, I was diagnosed with placenta previa and a two-vessel umbilical cord instead of the normal three… There was a higher chance of heart and kidney problems, as well as lack of oxygen and chance of still birth. We were sent to U of U for a second opinion with higher-tech imaging. Weeks before the appointment, my whole family was praying and very supportive, even though there was a lot of other stuff going on. The day of the appointment we found out that the placenta was already moving out of the way. The baby’s growth and development looked good and normal. There was only a two-vessel cord, but no other complications, and the baby was going to be just fine. I had to go in for weekly checkups to monitor the baby’s movement and have additional ultrasounds to keep track of the growth (i).”
Frequently Asked Questions
1. Does a two-vessel cord signify Down’s syndrome?
No, your uterus having a two-vessel cord does not necessarily mean your baby has Down’s syndrome. However, note that a two-vessel cord increases the risk of the baby experiencing fetal distress or developing Down’s syndrome. Therefore, adequate monitoring and tests are needed to determine the neonatal outcome and its management (5).
2. What does an infected umbilical cord look like?
An umbilical cord infection may adversely affect maternal health and will have the following symptoms (6):
- Red and inflamed cord
- Cloudy and foul-smelling discharge
- Minor bleeding
- Swelling in the area around the cord.
3. Can a two-vessel cord be treated or corrected during pregnancy?
There is no recorded evidence denoting a treatment or correction procedure for a single umbilical artery or a two-vessel cord.
4. Can a two-vessel cord affect future pregnancies for the mother?
There is no evidence to suggest that a two-vessel cord can affect future pregnancies in the mother. However, it’s best to consult your doctor before planning for the next pregnancy.
Some women may have a missing artery in the umbilical cord. If you have two blood vessels instead of three blood vessels in your umbilical cord during pregnancy, your doctor may keep you under observation. The doctor may diagnose the condition in the 18th week of pregnancy during routine scans. The condition may be more common in women carrying multiple babies or above 40 years of age. While most women with a two-vessel cord go on to have normal pregnancies, some might experience complications.
Infographic: Factors That Increase The Risk Of A Two-Vessel Cord
A two-vessel cord pregnancy may cause complications for the baby; hence an expecting mother with this condition needs constant monitoring and regular prenatal care. Nonetheless, some factors can make a pregnant woman more susceptible to developing a two-vessel cord, as highlighted in the infographic below. Illustration: Momjunction Design Team
Worried about your baby’s umbilical cord having only one artery? Find out if it’s of clinical importance in this video.
Personal Experience: Sources
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. A loss for words;https://pioneermom740863089.wordpress.com/2019/10/10/a-loss-for-words/
References
- Homeira Vafaei et al.; (2021); Prevalence of single umbilical artery clinical outcomes and its risk factors: A cross-sectional study.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8261099/ - Yajuan Xu et al.; (2016); Association Between Isolated Single Umbilical Artery and Perinatal Outcomes: A Meta-Analysis.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4913809/ - Shilpa Chetty-John et al.; (2010); Long-term physical and neurologic development in newborn infants with isolated single umbilical artery.
ttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC3454509/ - Cristina Martínez-Payo et al.; (2014); Detection of Single Umbilical Artery in the First Trimester Ultrasound: Its Value as a Marker of Fetal Malformation.
https://www.hindawi.com/journals/bmri/2014/548729/ - Helping you understand scary (but often harmless) pregnancy ultrasound findings.
https://utswmed.org/medblog/pregnancy-ultrasound-scary/ - Umbilical Cord Infection (Newborn).
https://www.fairview.org/ - Single umbilical artery.
https://radiopaedia.org/articles/single-umbilical-artery - Marina Basta and Brody J. Lipsett; (2023); Anatomy, Abdomen and Pelvis: Umbilical Cord.
https://www.ncbi.nlm.nih.gov/books/NBK557389/ - Umbilical cord conditions.
https://www.marchofdimes.org/find-support/topics/birth/umbilical-cord-conditions - Sandra Prucka et al.; (2004); Single umbilical artery: What does it mean for the fetus? A case-control analysis of pathologically ascertained cases.
https://www.nature.com/articles/gim20047 - Fırat Tülek et al.; (2015); Determination of risk factors and perinatal outcomes of singleton pregnancies complicated by isolated single umbilical artery in Turkish population.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4358306/ - Yu-Peng Wu et al.; (2014); Prenatal sonographic diagnosis of single umbilical artery: Emphasis on the absent side and its relation to associated anomalies.
https://www.sciencedirect.com/science/article/pii/S1028455914000709
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Subhashis Samajder
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das
















