Image: ShutterStock
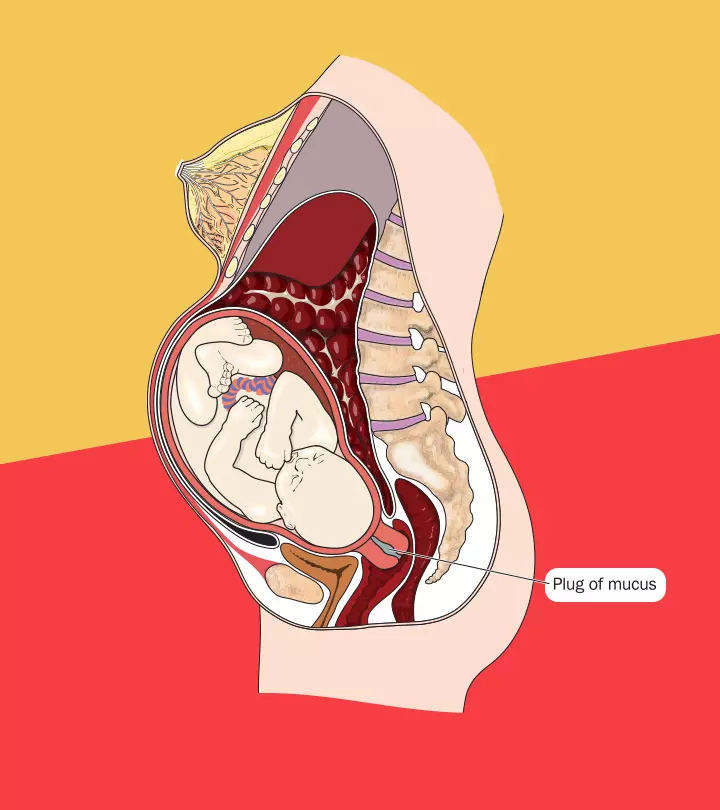
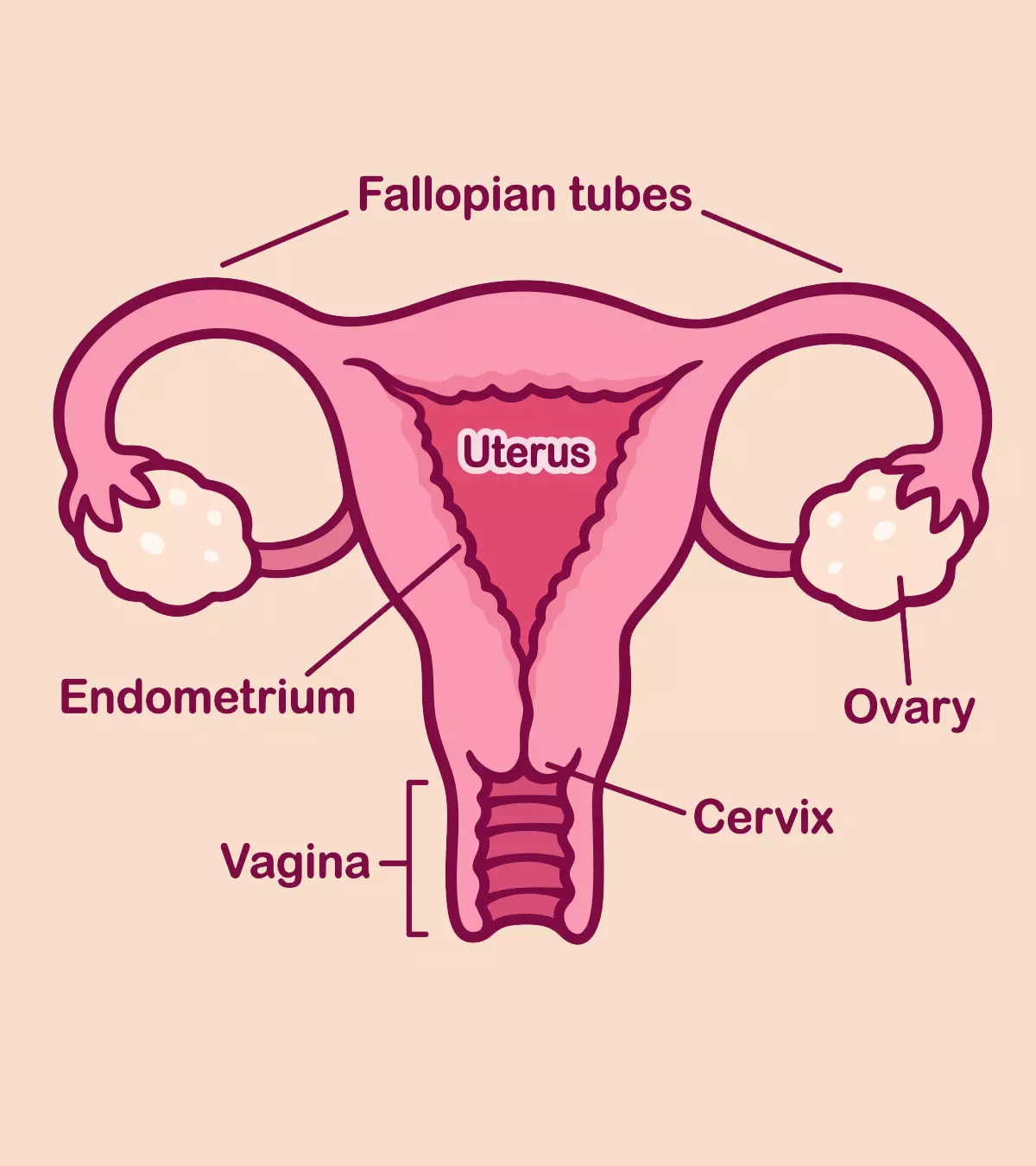
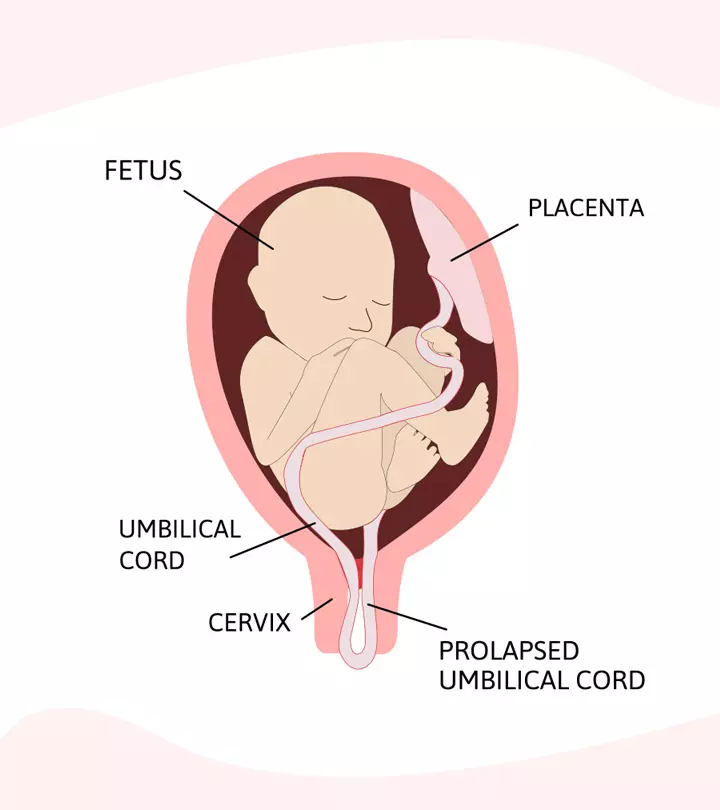
Umbilical cord prolapse is a condition where the umbilical cord drops through the open cervix to the vagina before the baby during or before birth. This is an obstetric medical emergency, and immediate delivery through cesarean section is usually recommended to avoid the risk of brain damage due to poor oxygenationi Oxygen supplementation of any system, including the human body .
The umbilical cord connects the mother and the baby. The three umbilical blood vessels carry blood, oxygen, and nutrients to the babies. So, cutting the cord from the baby before birth can be life-threatening. Read on to know the causes, complications, and other factors related to umbilical cord prolapse.
Key Pointers
- Umbilical cord prolapse is when the cord pushes into the birth canal before the baby.
- It may be caused due to premature rupture of membranes or multiple deliveries, which may affect the flow of oxygen to the baby’s brain.
- If you have a prolapse at home, call for emergency help.
- To prevent a prolapse, avoid lifting heavy weights and cervical checks.
What Is A Cord Prolapse?
Cord prolapse happens when the umbilical cord drops through the cervix and pushes into the birth canal before the baby.
It gets trapped against the baby’s body, thereby blocking the blood and oxygen supply. Cord prolapse could be an obstetric emergency that can affect the baby’s health (1).
Umbilical cord prolapse is likely to occur in one out of 500 pregnancies (2).
Types Of Cord Prolapse
Cord prolapse can be overt or occult, depending on the baby’s birth positions.
- Over prolapse is when the cord drops through the cervix or vagina before the presenting part (head) of the baby is visible or felt by the doctor. This is a very common type of umbilical cord prolapse.
- Occult prolapse occurs when the cord drops along with the presenting part of the baby. It usually happens in the case of intact or ruptured membranes (3).
In both types, immediate delivery is required to prevent fetal distressiSigns during pregnancy or childbirth that indicate that the fetus has inadequate oxygen or nutrition .
Signs And Symptoms Of A Cord Prolapse
Considering that a cord prolapse occurs during or before delivery, doctors will check for the following signs to diagnose it:
- Feeling or seeing the cord before the baby is the most apparent sign of cord prolapse.
- Fetal distress that causes decreased heart rate due to lack of oxygen. The drop in the fetal heart rate is detected through the fetal monitor (4).

Image: Shutterstock
- These signs may indicate complications during delivery, requiring emergency obstetric care.
- Most of the time, it precedes the spontaneous rupture of the membrane or succeeds in its artificial rupture.
Causes Of Cord Prolapse
Several factors could lead to cord prolapse. Some of them are (4):
- Premature rupture of the membranes (PROM): The amniotic sac could sometimes rupture too early or when the doctor performs amniotomy (procedure to accelerate labor). In these cases, when the baby’s head is too high in the uterus, the cord emerges first. The cord will then get compressed as the baby follows.
- Polyhydramnios (excessive amniotic fluid): If there is an excess of amniotic fluid, the pressure of the fluid pushes out the cord forcefully before the baby.
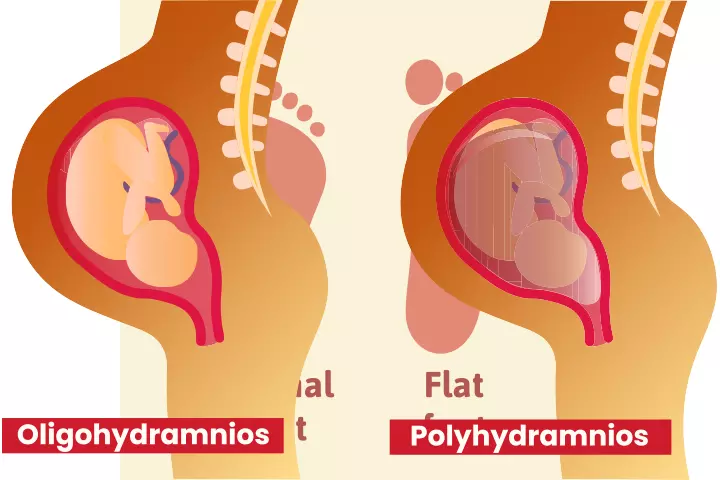
Image: Shutterstock
- Delivering multiples: In the case of twin babies or triplets, the first baby, while exiting, may push out the cord of another baby.
- Malpresentation of the baby: A breech position is one of the unusual delivery presentations where the baby’s feet come out first, giving space for the cord to come out of the birth canal beforehand. Also, the side lie (transverse) position or oblique lie might cause the cord to come out first.
- Premature delivery: The small fetal size combined with more amniotic fluid can trigger the cord to exit first.
- Long cord: An umbilical cord that is longer than usual might also cause a prolapse.
- Funic presentation: A variation in the cord position where it is pointing towards the internal cervical opening or lower uterine segment.
The other risk factors associated with umbilical cord prolapse include:
- Labor interventions like manual rotation of the fetal head
- Low birth weight
- Marginal insertion of cord, where it inserts into the edge of the placental disciFormed by maternal and fetal tissues to create a specific barrier that helps in the exchange of gases and nutrients without contact
- Uterine fibroidsi Non-cancerous tumors made of muscle and connective tissue that grow in the uterine wall of a woman of childbearing age or muscle tumors of the uterus
- Congenital uterine abnormalities such as septate, bicornuate, arcuate, unicornuate and didelphys uterusiA congenital condition where a woman has two uteruses .
- Cephalopelvic disproportion (baby’s head or body is too large)
- Placenta previa (low-lying placenta)
Complications Of Cord Prolapse
A cord prolapse could lead to the following complications (2):
- The fetal heart rate changes with cord compression, resulting in variable deceleration (irregular and jagged dips in fetal heart rate).

Image: Shutterstock
- Changes in blood pressure due to lack of oxygen and changes in heart rate.
- Respiratory acidosis occurs when the umbilical cord vein compresses, causing carbon dioxide to accumulate in the baby’s blood.
- Prolonged cord compression will further affect the flow of blood and oxygen to the baby’s brain.
- It can cause short bouts of fetal hypoxia (lack of oxygen in the womb), leading to fetal death.
How Is Umbilical Cord Prolapse Diagnosed?
The diagnosis of cord prolapse involves (4):
- Detecting the baby’s heart rate using a fetal heart monitor. In the case of cord prolapse, the baby’s heart rate goes down to less than 120 beats per minute.
- Pelvic examination to see or feel the cord using fingers.
- Cord prolapse could be detected with an ultrasound before delivery. This is especially important in the case of fetus’ malpresentation, multiple births, known as placental abnormalities.
What Can You Do If You Have A Cord Prolapse At Home?
Since cord prolapse leads to the risk of oxygen and blood deficiency to the fetus, it should be dealt with at the earliest. But how do you know if it is a cord prolapse?
First, your water breaks, and you will feel that there is something (cord) in your vagina. In such a case, call for medical assistance as it is an obstetric emergency and take the following measures until help arrives.
- With your partner’s help, remove the pressure off the cord by holding the presenting part up gently. Do not touch the cord as it may cause vasospasmiNarrowing of the arteries due to abrupt contraction of their muscular walls .
- With the cord compression, the oxygen supply to the baby is minimal. In this case, remain calm and take deep breaths to supply your baby with as much oxygen as possible.
- While you wait, get on all the fours to take off the pressure from the cord (5).
- You may also adopt knee-chest position or left lateral position by placing a pillow under the left hip.
 Caution
CautionCord Prolapse Management And Treatment
Your medical practitioner or obstetrician will first ask you to move into a comfortable position at the hospital.
The standard treatment is to encourage immediate delivery through the quickest and safest way possible. It involves c-section, especially when you are in early or preterm labor. Vaginal delivery might be attempted if it is considered safe.
Other treatment interventions required to reduce the cord compression and lower the risk of fetal complications include:
- Manually elevating the presenting fetal part through digital vaginal examination.
- Filling the bladder with normal saline using a urinary catheter, to elevate the fetal part.
- Moving the mother to a left lateral position, with the head down and feet elevated on pillows.
- Giving tocolytics (medications that suppress labor) for uterine relaxation and to prevent contractions.
If the fetal heart rate is stable, the doctor might go for category 2 LUCS. But if the heart rate pattern is non-reassuring, they may go for immediate LUCS with verbal consent.
Whitney Gorman, a stay-at-home mom of three children, vividly recounts the experience of encountering cord prolapse during her labor. She reflects, “The nurse, who had been incredibly helpful, was waiting with me. She informed me that my baby had a prolapsed cord, which essentially means the cord is attempting to emerge before the baby’s head …The procedure for this condition involves inverting the bed so that I was lying with my head lower than my feet. They attempted to adjust the bed in this manner, but it was stuck and wouldn’t budge. Consequently, they had to resort to emergency surgery to swiftly deliver the baby (i).”
Can Cord Prolapse Be Prevented?
There are no definite methods to prevent umbilical cord prolapse, but there are some things you can do to lower the risk of this complication.
- Avoid cervical checks as they carry the risk of accidental rupturing of the membranes.
- Avoid lifting heavy weights and indulging in vigorous physical activities that could lead to the water breaking before it is time for natural labor.

Image: Shutterstock
- If the situation demands labor induction, go for a c-section as it is a safer alternative.
- If you are aware of conditions such as polyhydramnios or fetal positioning, prepare in advance for any risks.
Frequently Asked Questions
1. What is the survival rate of cord prolapse?
A study conducted over 20 years and published by the National Library of Medicine stated that the risk of perinatal mortality was 7% with cord prolapse. The rate of survival might increase with surgical intervention. Hence, it is advisable to visit a hospital (6).
2. What is the difference between umbilical cord prolapse and cord presentation?
During an umbilical cord prolapse, the baby’s umbilical cord descends through the cervix into the vagina by rupturing the membranes. Cord or funic presentation occurs when the cord moves between the fetus and the cervix with or without rupturing the membranes (7).
3. Can the cord prolapse before the water breaks?
The umbilical cord prolapse may occur before the water breaks in rare cases. It is considered an obstetric emergency and requires immediate medical intervention (8).
4. What are the potential long-term effects on a baby born with umbilical cord prolapse?
With timely interventions, most babies may not suffer long-term effects. However, they are prone to brain damage (birth asphyxia) in extreme circumstances due to a significant lack of oxygen (8).
5. How does the timing of umbilical cord prolapse affect the outcome for the baby?
Without prompt medical intervention, cord compression can lead to fetal hypoxia. If the condition is identified and treated immediately, fetal disability or mortality rates can be reduced (9).
The risks of umbilical cord prolapse can be reduced through continuous fetal monitoring of movements and positions during the later stages of pregnancy. If you experience any discomfort or are sure that the cord is out of your vagina, contact your doctor immediately. Then, try to reduce the pressure on the cord by getting down on your fours. You should also avoid lifting heavy weights and going for cervical checks during pregnancy since it might increase the risk of cord prolapse.
Infographic: Reasons For Umbilical Cord Prolapse
Umbilical cord prolapse is a rare pregnancy complication that can put the mother and the baby at risk. Understanding the possible causes is crucial for early detection and appropriate management of this condition. Check out the infographic below to learn about common causes that can lead to umbilical cord prolapse in pregnancy. Illustration: Momjunction Design Team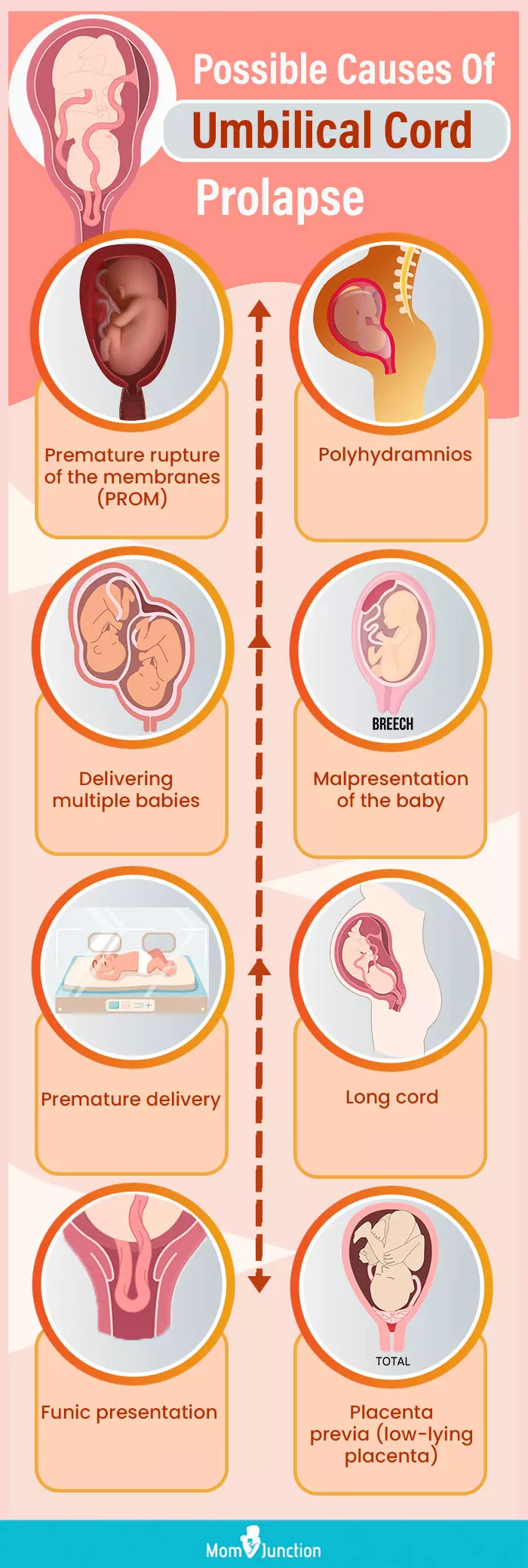
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Birth story | Emergency C-section | Prolapsed cord;https://www.youtube.com/watch?v=LtbsWSry1JQ&feature=youtu.be
References
1. Umbilical Cord Prolapse.https://www.ncbi.nlm.nih.gov/books/NBK542241/
2. Marybeth Lore, MD; Umbilical Cord Prolapse and Other Cord Emergencies; The Global Library Of Women’s Medicine (2017)
3. E. W. Wasswa et al.; Fetal demise and associated factors following umbilical cord prolapse in Mulago hospital, Uganda: a retrospective study; Reprod Health (2014)
4. W. Ali Sayed Ahmed and M. Ahmed Hamdy; Optimal management of umbilical cord prolapse; Int J Womens Health (2018)
5. Umbilical cord prolapse in late pregnancy; RCOG
6. Mark P. Hehir et al.;Perinatal Death Associated With Umbilical Cord Prolapse; National Library of Medicine (2017)
7. Umbilical Cord Prolapse; RCOG
8. Umbilical cord prolapse in late pregnancy – patient information leaflet; Royal College Of Obstetricians and Gynecologists
9.Marina Boushra et al.;Umbilical Cord Prolapse; StatPearls; National Library of Medicine
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Subhashis Samajder
Read full bio of Rebecca Malachi
Read full bio of Dr. Ritika Shah
Read full bio of Reshmi Das