Image: Shutterstock
The placenta is a specialized organ that develops in pregnant women. It plays a critical role in protecting and nourishing the growing fetus. The presence of blood clots in the placenta during pregnancy may indicate some underlying health issues. For example, people with obesity are at a greater risk of clots. A clot forms when blood coagulates to form a mass or lump. Clotting is a natural mechanism to stop bleeding and aids the healing process. The placenta carries oxygen and nutrients to the fetus via blood and removes waste from it. Therefore, clots can interrupt its proper functioning. Keep reading this post as we discuss the causes of clot formation in the placenta and the various treatment options.
Key Pointers
- Blood clots in placenta can be caused by various factors and may restrict the delivery of oxygen and nutrients to the fetus.
- Certain medical conditions, such as high blood pressure, diabetes, obesity, and a history of blood clots, may increase the risk of blood clots in the placenta.
- Small blood clots present in the placenta may not cause any harm to the fetus; but large placental abruptions (causing blood clots) can be dangerous for the fetus.
- Placental abruption may present with symptoms such as intense pain and vaginal bleeding.
- Early detection and proper treatment can help avoid complications during pregnancy and delivery.
Causes And Risk Factors For Blood Clots In Pregnancy
Any problems in the placenta can become a cause of concern for your baby and may also lead to fetal death. Blood clots restrict the flow of oxygen and proper nutrients to your baby. Fetal hypoxia, or insufficient oxygen supply to the fetus, can be a direct consequence of placental blood clots and can lead to a range of developmental abnormalities.
Blood clots in the placenta may also prevent the flow of waste from your baby to you. Small blood clots may disappear on their own and may not affect your fetus in any way. However, in some cases, blood clots in the placenta may contribute to maternal mortality.
Here are the factors that can lead to the development of blood clots in placenta during pregnancy (5) (6):
1. Placental abruption may result in placental blood clots. This abruption may be complete separation or partial separation of your placenta from your uterus before your baby is born. In case of a placental abruption, you may suffer from abdominal pain or vaginal bleeding. If the abruption is small, you may not experience any symptoms. However, a large abruption can threaten fetal life due to blood loss.As per the data published in March of Dimes, about one percent of all pregnancies have placental abruption (7).
A study analyzing 1.45 million live births among patients aged 13 to 45 found that younger expectant mothers exhibit lower rates of venous placental abruption. In contrast, the rates are higher among older expectant mothers. The graphical representation provided below illustrates this trend for better understanding.

Rates of Placental Abruption by Maternal Age
Source: Risk of Pregnancy Complications Also a Concern for Younger Patients
2. Increasing maternal age over 35 years can increase the risk for thromboembolismiA condition where blood clots form in the pelvic area and travel to the heart or lungs , causing placental blood clot risks.
3. Being overweight, obese, or smoking regularly may also result in blood clots in the placenta.
 Did you know?
Did you know?4. Thrombophilias or clotting disorder can result in blood clots in pregnancy. This form of blood clot is generally inherited. Chances of miscarriage are very high in this case.
5. Diabetes and preeclampsia during pregnancy can increase the risk of complications related to blood clots in the placenta. These conditions arise in pregnancy or are pre-existing.

6. Infections and malignancies (cancers) cause an increased tendency for blood clotting.
7. Previous history of blood clots, c-sections, or hormone treatments can lead to clots.
8. Increased immobility due to any reason may increase placental blood clot risks.
 Point to consider
Point to considerIf you have been diagnosed with blood clotting disorder before, you need to take thinner blood like Heparin or Lovenox for your future pregnancies. Dr. Alan Lindemann, obstetrician and maternal mortality expert from North Dakota, says, “There are some clotting disorders which, until recently, have universally caused recurrent miscarriages. Many of these pregnancies don’t go past eight or nine weeks. The good news for these patients is that medications like Lovenox, one shot daily, will allow pregnancies to go to term healthily.”
Treatment Procedures For Blood Clots In Placenta During Pregnancy
Your healthcare provider shall probably opt for an ultrasound, genetic testing, or a physical examination in case of a blood clot in your placenta. Here is what the doctors suggest (6) (7):
- Anticoagulants: Mothers with clotting disorders may be prescribed blood thinning medication to prevent the existing clots from getting bigger. Life-threatening clots may be removed with a catheter or vein filter.
Lisa, a mother and blogger, tested positive for a genetic mutation (prothrombin or a factor 2 mutation) and was put on blood thinners. Sharing her experience, she says, “Being pregnant does put you at a slightly higher risk for a blood clot but now we know there was an underlying genetic factor contributing to the issue. Now I will need to stay on blood thinner injections for 5 months postpartum- I would have only had to stay on them for 2 months if the genetic testing all came back negative. Luckily I can drop down to 1 injection after the baby is born (I currently do 2 injections a day)… After reading more about the mutation, we are so thankful that the baby has done fine as people with this mutation have a significantly greater risk of miscarriages and stillborn babies (i).”
- Labor induction or C-section: In case of placental abruption, your doctor may suggest a C-section or induced labor. Mothers experiencing severe placental abruption suffer from huge blood loss and the babies face complications from oxygen deprivation or preterm birth, requiring the baby to be delivered as soon as possible.
- Hospitalization: When placental abruption is not very severe, there is no immediate risk posed for the mother or baby. Mothers are generally hospitalized and kept under observation in this case. Bleeding generally stops after some time and the baby gets delivered from 24 to 34 weeks.

- Steroids: The baby may be prescribed steroids to help lung development and improve his or her chances of survival. Post-treatment and regular follow-up appointments with your healthcare provider are essential to monitor the condition and ensure maternal and fetal health.
- Lifestyle changes: You may be referred to a dietician who may prescribe a balanced diet with adequate hydration to help manage weight gain. The doctor may also provide an exercise regime and frequent movement to prevent further clotting issues. You may also be encouraged to quit harmful habits such as smoking and drinking.
Frequently Asked Questions
1. Can I have a healthy pregnancy with blood clots?
Under proper medical guidance and supervision, most women with blood clotting conditions go on to have healthy pregnancies. However, these conditions may cause issues for some women. Thus, women with a history of blood clots should maintain a healthy lifestyle and follow suggested treatment (1).
2. What do miscarriage blood clots look like?
The appearance of miscarriage blood clots can differ based on the pregnancy stage. For instance, at six weeks, women may notice blood clots with a small fluid-filled sac. The embryo might also be seen inside the sac but not clearly. However, the blood clots at eight weeks may look dark red and shiny with an embryo about the size of a bean (2).
3. How can I reduce or prevent the risk of blood clots in the placenta?
Following a healthy lifestyle, staying physically active, avoiding smoking, and knowing your family history are a few ways you may prevent blood clot formation during pregnancy. Wearing loose clothing, maintaining a healthy weight, avoiding prolonged periods of immobility, and staying hydrated can also help. Also, consider taking all the medications that you are prescribed and discuss the appropriateness of wearing belly support belts with your doctor (1) (3) (4).
Blood clots in the placenta during pregnancy might be caused by various factors, including infections, high blood pressure, and diabetes. However, this condition should be treated immediately to avoid complications during pregnancy or delivery. If you notice vaginal bleeding or abdominal pain, they could be signs of placental abruption. It is advised to consult your doctor immediately under such circumstances to receive the necessary treatment. If the placental abruption is not severe and does not pose risks to the mother or fetus, the doctor may recommend keeping the mother under observation.
Infographic: Preventing Blood Clots During Pregnancy
One potential complication that may arise during pregnancy is the formation of blood clots. They can form in the legs or lungs, which can be dangerous for the mother and the developing baby. So here are the steps pregnant women can take to help prevent the formation of blood clots during pregnancy. Illustration: Momjunction Design Team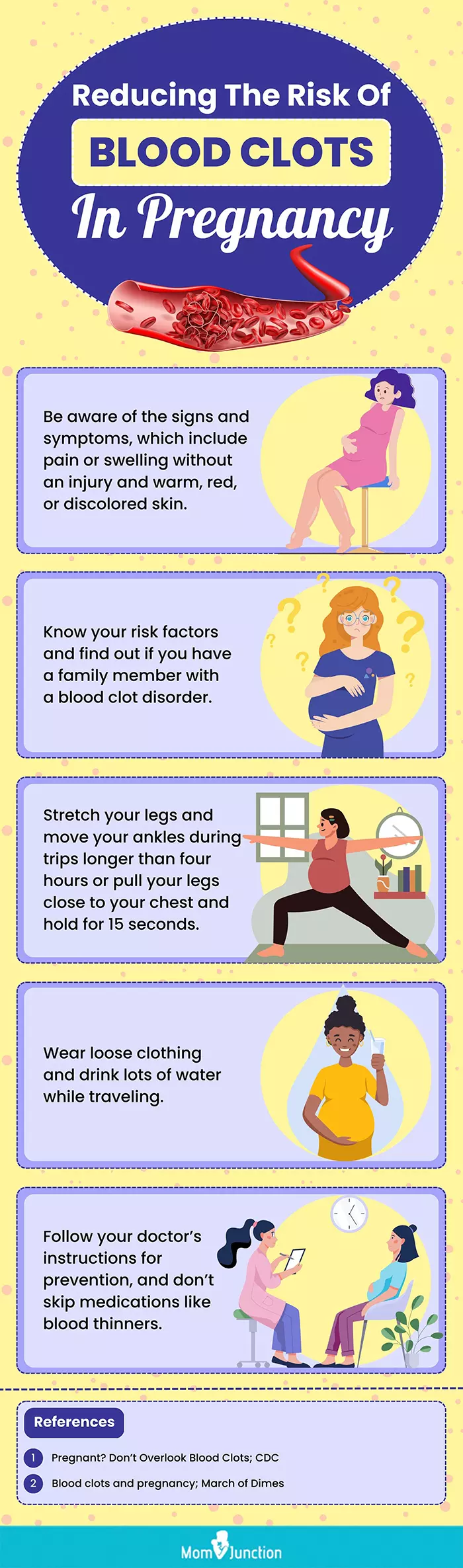
Personal Experience: Sources
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. 5 Things Friday!;https://lisasyarns.blogspot.com/2018/02/5-things-friday.html
References:
- Blood Clotting & Pregnancy.
https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=90&ContentID=P02437 - What Really Happens During A Miscarriage.
https://www.pregnancybirthbaby.org.au/what-really-happens-during-a-miscarriage - Blood Clots In Placenta During Pregnancy.
https://www.birthinjuryhelpcenter.org/birth-injuries/prenatal-problems/blood-clots-pregnancy/ - Your Guide to Preventing and Treating Blood Clots.
https://www.ahrq.gov/patients-consumers/prevention/disease/bloodclots.html - Blood Clotting & Pregnancy.
https://www.hematology.org/education/patients/blood-clots/pregnancy - Blood Clots During Pregnancy: Symptoms & Risks.
https://unmhealth.org/stories/2023/05/blood-clots-during-pregnancy-symptoms-and-risks.html - Placental abruption.
https://www.marchofdimes.org/find-support/topics/pregnancy/placental-abruption
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Meenu Vashisht Ahuja
- Dr. Alan Lindemann is an obstetrician and maternal mortality expert, who worked as a clinical associate professor at the University of ND. An alumnus of the University of ND and the University of Minnesota, he is a member of the American College of Obstetricians and Gynecologists and the American Medical Association.
 Dr. Alan Lindemann is an obstetrician and maternal mortality expert, who worked as a clinical associate professor at the University of ND. An alumnus of the University of ND and the University of Minnesota, he is a member of the American College of Obstetricians and Gynecologists and the American Medical Association.
Dr. Alan Lindemann is an obstetrician and maternal mortality expert, who worked as a clinical associate professor at the University of ND. An alumnus of the University of ND and the University of Minnesota, he is a member of the American College of Obstetricians and Gynecologists and the American Medical Association.
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das