Image: Shutterstock
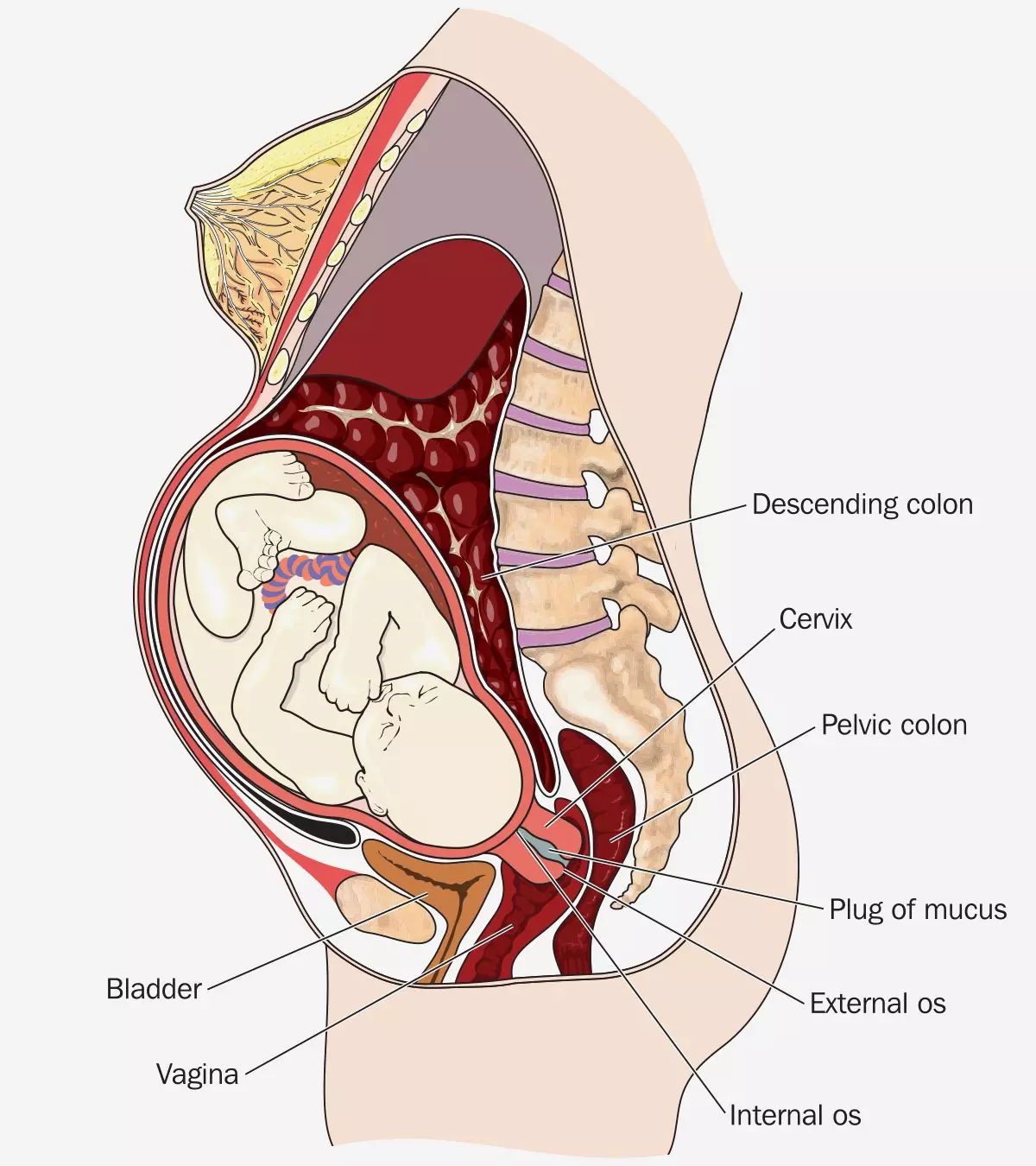
Uterine prolapse during pregnancy is rare, with an estimated incidence of one in every 10,000 to 15,000 deliveries. Usually, ligaments and pelvic floor muscles hold the uterus and place it in its position. The weakening of muscles and ligaments due to damages or stretching can cause prolapse, dropping the uterus into the vagina (1) (2). The treatment is planned according to the degree of prolapse. Read on to know the causes, signs, and treatment of uterine prolapse in pregnancy and its complications.

Key Pointers
- Uterine prolapse happens when the pelvic floor muscles become weak due to damage and stretching.
- Previous pregnancies and deliveries may increase the risk of uterine prolapse.
- Back pain, pelvic heaviness, or visible protrusion from the vagina are some symptoms of uterine prolapse.
- Kegel exercises, avoiding heavy weight lifting, a good diet, and moderate physical activity can help prevent uterine prolapse.
- Early diagnosis and proper management are crucial for a safe pregnancy and delivery.
Effect Of Uterine Prolapse On Pregnancy
A prolapsed uterus during pregnancy can lead to various complications that may affect both the mother and the baby. Early diagnosis and management are crucial to prevent severe outcomes. Below are some potential complications associated with uterine prolapse during pregnancy (2) (3).
- Preterm labor: The added pressure on the uterus may trigger early contractions, increasing the risk of premature birth (4).
- Difficulty during labor and delivery: A prolapsed uterus can obstruct the birth canal, making vaginal delivery challenging and sometimes requiring a cesarean section.
- Cervical discomfort: The cervix may become irritated or inflamed due to its abnormal positioning, leading to pain and discomfort.
- Cervical desiccationi and ulceration: Prolonged exposure of the cervix to external elements can cause dryness and ulcer formation, increasing the risk of infections (5).
- Urinary tract infection: The displacement of the uterus can put pressure on the bladder, leading to incomplete emptying and an increased risk of bacterial infections (5).
- Acute urinary retention: Severe prolapse may obstruct the urinary tract, making it difficult to urinate (4).
- Fetali and maternal sepsis: Infections resulting from prolapse-related complications can spread, leading to life-threatening conditions for both the mother and baby.
- Postpartum hemorrhagei : Weak pelvic floor muscles may contribute to excessive bleeding after delivery, requiring immediate medical attention (4).
Complex cases of uterine prolapse may cause abortion of the fetus. Complications may occur even after childbirth (6). But do not panic since extreme complications and problems due to uterine prolapse usually occur when the condition is ignored. The symptoms of uterine prolapse seldom go unnoticed, and you are likely to feel it before the problem gets worse.
Signs And Symptoms Of Uterine Prolapse During Pregnancy
Uterine prolapse can present with various symptoms that may range from mild discomfort to severe complications. Early recognition of these signs can help in managing the condition effectively. Here are some common symptoms of uterine prolapse during pregnancy (7)(8):
- A visible protrusion from the vagina. In more advanced cases, part of the uterus may descend so much that it becomes visible outside the vaginal opening.
- Sensation of a bulge in the vagina. Some women may feel a heaviness or the presence of a lump in the vaginal canal, even if there is no external protrusion.
- Pelvic heaviness
- Pressure, heaviness, and a dragging sensation in the vagina
- Back pain
- Urinary incontinence – the feeling of incomplete emptying
- A feeling of incomplete emptying of the bowel
The symptoms of uterine prolapse are usually most noticeable during the third trimester. See a doctor for antepartum care if you notice or feel the symptoms.
Prolapse is unlikely to be present before pregnancy. If present, it may resolve during pregnancy but may reappear after childbirth (6).
Recalling her experience with a postpartum uterine prolapse, Dr. Brianne Grogan, a mother and a doctor of physical therapy, says, “I was running, and I felt a, what I want to describe it as is kind of a pop. Although it certainly wasn’t that dramatic, it was a definite change in my pelvic region. I felt a drop, and I felt again what I can only describe as a pop. Although it wasn’t like a snap, it was a feeling of a drop. And I went home, and I thought oh my God, I have developed a prolapse (i).”
Causes Of Uterine Or Cervical Prolapse During Pregnancy
Pelvic muscles may weaken due to several reasons and increase the chances of uterine prolapse. The following conditions and factors may increase the risk of developing uterine prolapse (2)(6)(9).
- Trauma to the pelvic muscles during vaginal childbirth may stretch and weaken the muscles. It increases the chances of developing uterine prolapse in subsequent pregnancies.
Jessica Valant, a Pilates teacher and women’s health instructor, shares her experience with uterine prolapse after childbirth and its effects on her health. She says, “I was also diagnosed with a prolapse after the birth of our first child… My symptoms included a constant bulge out of my vagina, pelvic pain and pressure, and some bloating. I also continued to have endometriosis symptoms and pain (ii).” - Multiple pregnancies and multiple deliveries, like in the case of delivering twins or triplets.
- Delivering a large baby through vaginal birth.
- Subsequent pregnancies with short intervals could also make the uterus susceptible to prolapsing.
- Congenital connective tissue disordersiGenetic disorders that impact connective tissue development could cause pelvic muscles and ligaments to remain weak, which increases the chances of uterine prolapse.
- Physiological changes of the uterus, ligaments, and muscles of the body during pregnancy. For instance, hormonal changes during pregnancy could cause relaxation of ligaments. It may increase the risk of uterine prolapse.
- Chronic intra-abdominal pressure due to persistent straining for bowel movement or repeated lifting of heavy weights.
 Be watchful
Be watchfulYour doctor will determine the exact cause of uterine prolapse after performing diagnostic steps.
Diagnosing Uterine Or Cervical Prolapse During Pregnancy
Healthcare practitioners can diagnose the prolapse through pelvic examination. The doctor may ask the patient to perform a Valsalva maneuver, a breathing technique, which can help the doctor examine the full extent of the prolapse (10). The doctor may suggest an MRI of the pelvis to further confirm the diagnosis (11).
Treatment Of Uterine Or Cervical Prolapse During Pregnancy
The treatment approach depends on the stage of prolapse, the stage of pregnancy, and if the patient has any other complications. Your doctor may suggest the following treatment and care measures during pregnancy (12).
- Maintaining genital hygiene may help prevent the development of infections and other complications.
- Strengthening pelvic floor muscles can reduce uterine prolapse symptoms by providing better support to the uterus. A healthcare professional, such as a physical therapist, can guide you through targeted exercises like Kegels to enhance muscle strength (11).
- The doctor may place a small device called a pessaryiA device inserted into the vagina to provide support for the uterus, bladder, or rectum into the vagina to prevent the uterus from collapsing. The pessary is kept in place until the onset of labor.
 Things to consider
Things to consider- If other conservative treatment steps are ineffective, then the doctor may perform a laparoscopic uterine suspension where the uterus is surgically suspended back to its original position. If uterine prolapse persists even as you approach the due date, the doctor may consider obstetric interventions such as performing a cesarean section to prevent complications.
Prevention Of Uterine Prolapse During Pregnancy
There is no particular way to prevent uterine prolapse during pregnancy. Observing certain precautions and making some changes in lifestyle may help reduce the risk of developing uterine prolapse. The following are some ways you can take care of your maternal health to minimize the chances of developing uterine prolapse (11) (13).
- Lose weight if you are overweight
- Include fiber and fluids in your diet to avoid constipation or excessive straining
- Avoid lifting heavy weights
- Quit smoking
- Take medical advice in case you have chronic cough since it can strain pelvic organs and muscles
- In mild cases, you may perform Kegel exercises to strengthen your pelvic floor muscles. Make sure to discuss with your healthcare practitioner or physiotherapist before performing any exercise during pregnancy.
An existing uterine prolapse may resolve after childbirth, and there is also no risk to the baby after delivery.
Uterine prolapse may occur as a result of one factor or due to a combination of factors. It can be categorized into stages.
Stages Of Uterine Prolapse

There are different stages of uterine prolapse, depending on how far the uterus dropped into the vagina. The following are the four stages (7) (9).
- Stage I: The uterus drops down to the upper half of the vagina. The most distal portion of the prolapse is >1cm above the level of the hymen.
- Stage II: The uterus has dropped down nearly to the opening of the vagina. The most distal portion of the prolapse is ≤1cm proximal or distal to the hymen.
- Stage III: The uterus protrudes out of the vagina. The most distal portion of the prolapse is >1cm below the hymen but protrudes no farther than 2cm less than the total length of the vagina.
- Stage IV: The uterus is completely out of the vagina. There is a complete eversion of the vagina.
Chances Of Pregnancy And Natural Birth With Prolapsed Uterus
Early diagnosis, prompt treatment, careful monitoring throughout pregnancy, and proper management of the condition can lead to a safe pregnancy or gestation period (2). Various published case studies have reported successful natural birth with a prolapsed uterus (6) (8). However, in some cases, a cesarean delivery is suggested over vaginal delivery to prevent potential risks such as cervical lacerationsiA cervical tear that may happen during childbirth or obstructive labor (14).
Frequently Asked Questions
1. Does uterine prolapse increase the risk of miscarriage?
The complications arising from uterine prolapse during pregnancy could vary from cervical infection to a miscarriage. However, most cases of uterine prolapse are treated, resulting in successful vaginal delivery (15).
2. Does bed rest help uterine prolapse?
Bed rest is a crucial part of the uterine prolapse intervention strategy. Even though the treatment plan may vary per each woman’s condition, bed rest is a common suggestion for everybody (16).
3. Can uterine prolapse during pregnancy affect future pregnancies?
Uterine prolapse during pregnancy may recur during a future pregnancy. Therefore, doctors recommend inserting a pessary inside the vagina to ease the symptoms (17).
4. How does uterine prolapse during pregnancy affect delivery?
During delivery, a pregnant woman with uterine prolapse will likely experience inadequate cervical dilatation, cervical laceration, and obstructive labor. In severe cases, hysterorrhexis at the lower uterus, fetal death, and maternal morbidity could also be possible (6).
5. What is the difference between a uterine prolapse and a cystocele?
Cystocele is another type of prolapse in which the urinary bladder drops into the vagina, whereas, in the case of uterine prolapse, the uterus drops into the vagina (18).
6. Can I push up a uterine prolapse?
No, it is not advised to try and push your prolapsed uterine back up as it might lead to unknown complications. The only acceptable way to treat a prolapsed uterus is to visit your OB-GYN and receive the appropriate treatment (19).
7. Is it okay to walk with a prolapsed uterus?
Dr. Menka Gupta, Singapore-based medical doctor and healthcare entrepreneur, says, “Walking is generally considered a safe and beneficial low-impact exercise for women with uterine prolapse. However, it’s crucial to pay attention to your body, and if walking causes discomfort or increased pressure in the pelvic area, it’s important to listen to your body. Mild to moderate physical activity, including walking, usually benefits women with uterine prolapse. It can help maintain a healthy weight, reducing pressure on the pelvic floor muscles. Additionally, it aids in strengthening the pelvic floor muscles and decreasing the risk of symptoms. Alongside walking, I recommend pelvic floor exercises, such as Kegel exercises, to strengthen the muscles supporting the uterus, bladder, and rectum.”
Uterine prolapse during pregnancy may result in preterm labor, cervical discomforts, labor difficulties, urinary tract infection, fetal and maternal sepsisiA serious complication of an infection occurring during pregnancy, childbirth, or following an abortion , and postpartum hemorrhage. Some cases may result in pregnancy loss, such as miscarriage or stillbirth. A noticeable protrusion in the vagina, the sensation of a bulge in the vagina, back pain, pelvic heaviness, and pregnancy incontinence are some of the symptoms of uterine prolapse. Large babies, multiple pregnancies, trauma, congenital connective tissue disorders, and short intervals between pregnancies can increase the risk of uterine prolapse. Good hygiene practices, inserting pessaries into the vagina, or laparoscopic uterine suspension are done to manage uterine prolapse depending on the severity
Infographic: Aspects That Influence Treatment Choice For Uterine Prolapse
Healthcare providers recommend vaginal pessaries or surgery to treat uterine prolapse during pregnancy. This depends on various factors and expected outcomes in each woman. Read through the infographic to know the factors influencing the treatment choice for uterine prolapse during pregnancy.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Illustration: Uterine Prolapse During Pregnancy: Stages And Its Treatment

Image: Stable Diffusion/MomJunction Design Team
Uterine prolapse is a condition where the uterus drops down into the vagina. Learn about its causes, signs and symptoms, diagnosis and treatment in this video.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. My prolapse story (and how I fixed it);https://www.youtube.com/watch?feature=shared&v=jfapCYmcxMo
ii. Jessica Valant My story;
https://jessicavalantpilates.com/complete-hysterectomy-guide
References
1. Surgery for Pelvic Organ Prolapse: American College of Obstetricians and Gynecologists. (2018).
2. Buyükbayrak, E. E., Yılmazer, G., Ozyapı, A. G., Kars, B., Karşıdağ, A. Y., & Turan, C. Successful management of uterine prolapse during pregnancy with vaginal pessary: a case report: Journal of the Turkish German Gynecological Association, 11(2), 105–106. (2010).
3. Tsikouras, P., Dafopoulos, A., Vrachnis, N., Iliodromiti, Z., Bouchlariotou, S., Pinidis, P., … & Von Tempelhoff, G. F. Uterine prolapse in pregnancy: risk factors, complications and management: The Journal of Maternal-Fetal & Neonatal Medicine, 27(3), 297-302. (2014).
4. Ba’Abbad, Lina, et al., Uterine Prolapse in a Term Pregnancy: A Case Report.” Case Reports in Women’s Health,: vol. 41, 2025.
5. Uterine prolapse,: Mount Sinai.
6. Zeng, C., Yang, F., Wu, C., Zhu, J., Guan, X., & Liu, J. Uterine Prolapse in Pregnancy: Two Cases Report and Literature Review: Case reports in obstetrics and gynecology, 2018. (2018).
7. Doshani, A., Teo, R. E., Mayne, C. J., & Tincello, D. G. Uterine prolapse: BMJ (Clinical research ed.), 335(7624), 819–823. (2007).
8. De Vita, D., & Giordano, S. Two successful natural pregnancies in a patient with severe uterine prolapse: A case report. Journal of medical case reports, 5, 459. (2011).
9. Prolapsed uterus: Department of Health & Human Services, State Government of Victoria, Australia. (2017).
10. Pelvic Organ prolapse: American family Physician. (2010).
11. Uterine Prolapse: John Hopkins Medicine. (n.d.).
12. Latika, Nanda S, Chauhan M, Malhotra V. Pregnancy with third degree uterine prolapse-a rare case report.International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 5, 579-81. (2016).
13. What to do about pelvic organ prolapse: Harvard Health Publishing. (2014).
14. Daisuke Tachibana et al.; Successful Management of Uterine Prolapse in Pregnancy: A Case Report of Avoiding a Cervical Laceration by the Reduction of Massive Edema; Cureus; NCBI (2025)
15. Jeong Ok Kim et al; Uterine prolapse in a primigravid woman; US National Library of Medicine (2016).
16. Rakhi Gupta and Girija Tickoo; Persistent Uterine Prolapse During Pregnancy and Labour; US National Library of Medicine (2012).
17. Treatment; NHS
18. Surgery for Pelvic Organ Prolapse; ACOG
19. Uterine Prolapse; Cleveland Clinic
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sangeeta Agrawal
- Dr. Menka Gupta is a medical doctor and healthcare entrepreneur. She has graduated from the Institute Of Functional Medicine, Washington, and worked in ob/gyn at top hospitals in the UK, Singapore, and India.
 Dr. Menka Gupta is a medical doctor and healthcare entrepreneur. She has graduated from the Institute Of Functional Medicine, Washington, and worked in ob/gyn at top hospitals in the UK, Singapore, and India.
Dr. Menka Gupta is a medical doctor and healthcare entrepreneur. She has graduated from the Institute Of Functional Medicine, Washington, and worked in ob/gyn at top hospitals in the UK, Singapore, and India.
Read full bio of Dr Bisny T. Joseph
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das


















