Image: Midjourney/ MomJunction Design Team
Vomiting in toddlers may be distressing for parents, and things get even worse when your toddler is throwing up frequently. There are several reasons for your child’s vomiting, ranging from gastroenteritis (infection in the intestinal lining) to motion sickness. You may also find your toddler throwing up but with no fever. The cause of your toddler’s vomiting may not be clear at first, but if you take a closer look, you may find the actual cause. Understanding the underlying cause of your toddler’s vomiting is essential for addressing the issue effectively. If the toddler has persistent vomiting with no other symptoms, consult a doctor for professional advice. Read this post to figure out what’s causing your toddler’s vomiting, what you can do to manage it, and how to help prevent a repeat occurrence in your child.

Key Pointers
- The primary cause of vomiting among toddlers is gastrointestinal infection.
- Common symptoms that accompany vomiting include stomach pain, fever, and loose stools.
- Signs such as the presence of blood in vomit, high fever, diarrhea, green or black vomit, and a swollen abdomen require immediate medical attention.
- The treatment for vomiting in toddlers is subjective and depends on the underlying problem.
- Preventing vomiting can be aided by providing clean and hygienic food, limiting acid reflux, managing food allergies, avoiding motion sickness triggers, and keeping the child hydrated.
15 Causes Of Vomiting In Toddlers
Your child can feel nauseated and eventually vomit, due to several reasons. Here are the most common reasons why toddlers may vomit:
1. Stomach infection

Stomach infection is the leading cause of vomiting in toddlers, and among a plethora of stomach infections, viral gastroenteritis is the most common (1).
Viral gastroenteritis is also known as a stomach bug or stomach flu in toddlers. Food poisoning in babies is an infection that stems from contaminated or stale food. The infection causes severe stomach cramps resulting in excruciating pain in the abdominal cavity, which can lead to regurgitationiSpitting up of stomach contents without nausea or forceful abdominal contractions. of the stomach contents. It may cause the body temperature to rise, leading to fever with vomiting in toddlers. Fever is not always prevalent, though.
Symptoms: Vomiting could be accompanied by diarrhea, stomach upset, nausea, and fever. Diarrhea in toddlers may cause dehydration and result in a headache.
Treatment: Viral gastroenteritis generally gets better on its own with adequate home care and precautions. Parents must ensure the child takes sips of boiled and cooled water at regular intervals, especially after vomiting, to prevent dehydration. A doctor may suggest an oral rehydration salt (ORS) solution, which may be obtained from the pharmacy (1).
 Quick fact
Quick fact2. Intestinal infection
Your toddler may throw up when their intestines contract an infection. Numerous pathogensiAn organism or a germ responsible for causing diseases , bacteria, and viruses can infect the intestines and vomiting is a symptom of their presence in the body. Infections caused by bacteria, such as salmonellaiA bacteria that leads to salmonellosis, an infection characterized by fever, stomachache, and diarrhea. and staphylococcusiA bacteria that is found on the skin normally but has the potential to cause a wide range of minor or severe diseases , cause vomiting and diarrhea (2). Your kid may or may not have a fever.
Symptoms: Symptoms are the same as stomach infection viz. vomiting or gagging with diarrhea, upset stomach, abdominal cramps, and fever.
Treatment: Intestinal infections require blood and stool samples for testing. If diagnosed with a bacterial infection, the doctor may prescribe antibiotics to cure the illness and fluids to prevent dehydration. In severe cases with electrolyte imbalance, the toddler may require intravenous fluid replacement (2).
3. Appendicitis
Appendicitis is rare in infants and usually occurs in kids and teens aged between 10 and 20 years (3). An infected appendixiA small, finger-like pouch that's attached to the large intestine in the lower right abdomen could result in nausea and vomiting in toddlers, accompanied by excruciating pain in the abdomen, loss of appetite, and a low fever. The infected appendix sends pain impulses throughout the nerves of the abdominal cavity, which causes the stomach muscles to move abnormally, causing nausea and vomiting.
Symptoms: Piercing pain in the lower right side of the abdomen. There could be a constant sense of nausea, along with vomiting. The toddler may also develop a fever.
Treatment: Before beginning any treatment for appendicitis, the doctor may do a physical exam, test the toddler’s blood and urine, take abdominal X-rays, and conduct a few scans to determine the severity. In mild cases, the doctor may prescribe IV antibiotics followed by oral antibiotics for seven days. However, in severe cases, the antibiotic treatment may be followed by an appendectomyiA surgical procedure where the infected appendix is removed using a small device called a laparoscope. . In surgical cases, children are also provided with IV fluids and pain medication before discharge on the same day (3).
4. Pediatric hernia
A hernia happens when the bowel (small or large intestine) slips out of the abdominal cavity, causing discomfort and increasing the risk of infection. Toddlers can be affected by two types of hernia: inguinal hernia and umbilical hernia (4). An inguinal hernia occurs when the bowel moves into the inguinal canal leading to a swollen bump near the groin.
An umbilical hernia is when the abdominal wall right behind the navel is damaged, causing a portion of the small intestine to slip out of the damaged area. In either case, the hernia creates nerve pressure in the abdominal cavity, making the toddler throw up frequently.
Symptoms: Hernias are generally visible in the form of a bump in the lower abdomen or groin area. Symptoms apart from vomiting include constant nausea, abdominal cramps, and constipation.
Treatment: Prior to the treatment, the doctor may do a physical exam to see if the hernia is reducibleiA type of hernia which can be pushed back into the belly. . If not, the toddler may require an x-ray or ultrasound scan to determine whether it is an inguinal or umbilical hernia. Inguinal hernias require immediate surgery to put the intestine back into the abdomen and prevent damage from lack of blood supply. Umbilical hernias tend to close on their own by the time the child turns five years old. However, a doctor may suggest surgery, if the hernia seems to grow with age, is not reducible, or persistent beyond three years of age (4).
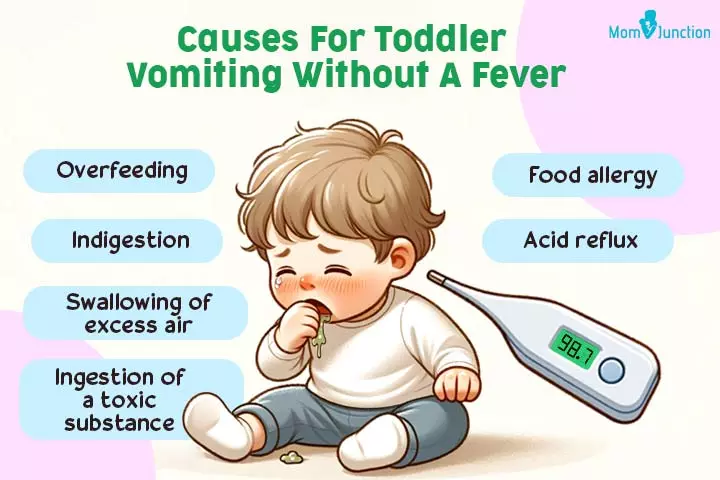
5. Ingestion of toxic substance
Toddlers tend to put things in their mouths. Vomiting could be the result of putting toxic substances, right from wild plants to soaps and detergents, in their mouth. These substances irritate the stomach lining, causing the muscles to contract and expel the contents (5). In the case of ingestion of toxic substances, the toddler may vomit but have no other symptoms such as fever or diarrhea.
Symptoms: In this case, symptoms are subjective and depend on the potency and quantity of the toxic substance consumed by the toddler. Vomiting could generally be accompanied by nausea and abdominal pain.
Dr. Lauren Chiriboga, a board-certified pediatrician from Nicklaus Children’s Hospital in Miami, Florida, says, “The first thing you should do is assess your child for the development of any new signs or symptoms, such as loss of consciousness, difficulty breathing, or change in mental status. If any of these are present, call 911 immediately. If your child has no concerning signs or symptoms, it is important to call Poison Control. Next steps may include observation at home or the recommendation to bring your child to the nearest emergency department if intervention is needed.”
Treatment: The first step before treatment would be to understand what poison has been ingested by the child. This is determined by a doctor by asking for medical history, blood testing, and administering either electrocardiogram, x-ray, CT scan, or MRI scan. Once diagnosed, the doctor may use different procedures such as orogastric lavageiA procedure in which a tube is passed into the stomach through the mouth, fluid is instilled, and then suctioned back out. or whole-bowel irrigationiA procedure where a tube is passed into the stomach through the mouth or nose and an electrolyte solution flushes the contents of the GI tract until clear fluid exits the rectum. (6) (7).
6. Food allergy
If your toddler is puking, usually after eating a particular food, then they may be allergic to that food. According to the National Health Interview Survey, food allergies are found in about 4.4 percent of all children aged zero to five years (8). Vomiting is one symptom of food allergies in babies (9). Throwing up white chunks of milk is a sign of milk allergy or lactose intolerance. Lactose intolerance is the inability of the small intestine to digest milk due to a shortage of the enzyme lactase, which is necessary for milk digestion. Other common food allergies are caused by eggs, peanuts, soy, wheat, tree nuts (walnuts, pistachios, pecans, cashews), and fish (salmon, cod, tuna, shellfish) (10).
Pediatrician Dr. Raashid Hamid says, “FPIES (food protein-induced enterocolitis syndrome), a non-IgE food allergy, causes severe vomiting two to four hours after ingesting trigger foods such as rice and oats. It’s often misdiagnosed as viral gastroenteritis. A detailed food diary and supervised oral food challenges are essential for diagnosis.”
Symptoms: Vomiting is one of the many symptoms of a food allergy. Other symptoms could be abdominal pain, skin hives, and swollen lips and eyelids.
Treatment: A board-certified allergist may conduct skin-prick tests, blood tests, or an oral food challenge to identify the primary allergen. This helps them determine the family of the allergen and the foods that the toddler may have cross-reactivity with. Once diagnosed, the first advice from the doctor would be to avoid the allergen. They may also prescribe an epinephrine auto-injector for emergencies when the child has anaphylaxis and teach you ways to use it. However, despite the administration of the shot, the child will require further emergency care at a hospital (9).
 Quick fact
Quick fact7. Acid reflux and bile reflux
Acid reflux occurs when the esophageal sphincter, between the esophagus and stomach, opens abnormally and lets some of the stomach’s contents, including acid, move upwards through the food pipe. The irritation caused by the acid to the esophageal lining causes nausea and vomiting (12).
Sometimes, the toddler might throw up bile, which is a greenish-yellow fluid. This is caused by bile reflux. Bile reflux happens when the pyloric valve between the stomach and small intestine malfunctions, allowing bile to move from the small intestine to the stomach. It then irritates the stomach lining, causing the muscles to contract and expel the bile in the form of vomit through the esophagus.
Acid reflux and bile reflux can be distinguished by the color of the expelled liquid. If the toddler has acid reflux and bile reflux together, then it becomes easier for the bile to come out of the stomach with the refluxed stomach acid.
Symptoms: Vomiting along with a burning sensation in the upper abdominal region and esophagus, and constant dull pain in the abdomen.
Treatment: After preliminary evaluations such as pH-testing, endoscopy, and bioscopy the doctor may suggest lifestyle and dietary changes such as avoiding high-fat foods, sleeping at an angle, losing weight, eating split meals, and wearing loose clothing around the abdomen. The doctor may also provide the child with age-appropriate doses of antacids, H2 blockers, proton pump inhibitors (PPIs), and prokinetics to aid digestion and prevent the discomfort (13).
8. Overeating and over-swallowing of air

Overeating or swallowing excess air during feeding can lead to vomiting (14). This may happen when the nipple of the feeding bottle has a big hole. The toddler may thus consume more milk than needed, causing their tiny stomach to fill to the brim and then throw up. Swallowing excess air due to poor positioning of the nipple in the mouth can also cause the toddler to have nausea and vomiting. Gulping down the milk or feeding too fast also causes the ingestion of air with food (15).
Symptoms: Along with vomiting, there could be a stomachache, and bloating in the abdomen area, with heavy burping.
Treatment: A doctor or lactation consultant may advise you to procure a bottle with a smaller hole in the nipple which can control the flow of milk. Ensure that the baby’s mouth makes a good latch around the nipple with no space for swallowing air. Also, sit the child upright after feeds and burp them before lying them down. Additionally, the weaning foods of the child must not include carbonated beverages, excessive citrus, fried or fatty foods, peppermint, chocolate, or caffeine. Parents must ensure that the child eats small or controlled portions of solid food at every meal to prevent overeating. The doctor may also prescribe over-the-counter antacids (16).
9. Indigestion
Indigestion can lead to vomiting due to the accumulation of undigested food in the stomach. The toddler may throw up undigested food hours after eating, indicating that the food has not been digested. This could happen when the little one has eaten the food too quickly, overeaten, or consumed extremely spicy or oily food.
Symptoms: Symptoms are subjective here. Generally, vomiting could be accompanied by pain in the stomach.
Treatment: A doctor may recommend lifestyle changes for indigestion. These will include eating split meals, chewing more, eating slowly, avoiding allergenic foods, and avoiding heavy activities or lying down immediately after meals. The child will also have to limit greasy foods, chocolates, caffeine, and citrus fruits. The doctor may also prescribe over-the-counter antacids and acid regulators (17).
10. Certain medication
Certain medicines could also make toddlers feel sick and vomit, especially if the toddler consumes them on an empty stomach. Vomiting can also be a known side-effect of some medicines.
Symptoms: Individual medicines have specific symptoms. Vomiting could be one of them.
Treatment: The treatment depends on the type of drug that has been ingested and the method of ingestion. When the child ingests tablets like aspirin, phenobarbital, or theophylline, doctors may use an activated charcoal solution. The child may either ingest this orally or have it administered through a nasogastric tube. Antidotes may be administered intravenously for certain medications like acetaminophen, digoxin, opioid painkillers, tricyclic antidepressants, and warfarin. The toddler may also need hyperbaric oxygen therapy if they have severe breathing difficulties. For other medications without antidotes and drugs available in the form of patches, syringes, or vials, doctors may use a drug and dose-specific treatment process after diagnosis (7).
11. Motion sickness and headaches
If your toddler has no symptoms or history of illness but suddenly throws up in a moving vehicle, then they may suffer from motion sickness. Motion sickness can be an indicator of vertigo, a condition where an individual feels the sense of a shifting balance. This happens when the toddler is in a situation (like a roller-coaster), where there is a constant shift of equilibrium and orientation.
This quick shift of balance overloads the inner ear, which is responsible for maintaining the body’s balance, and makes it send erratic signals to the brain (18). This disorients the brain, leading it to send distress nerve signals to the stomach muscles and making the toddler vomit. Other brain-related conditions, such as headaches, can also cause vomiting.
Symptoms: Dizziness, loss of balance, and a headache.
Treatment: The best way to address motion sickness in toddlers is to take adequate breaks and have the child look out the windshield instead of down. Doctors may advise the use of age-appropriate booster seats and prescribe an over-the-counter travel sickness medicine for toddlers over two years. Parents may also lie the child down with a cool washcloth over their forehead when they feel too sick. It is also essential to ensure that the child stays hydrated during travel, especially if they vomit (18).
12. Ear infections
Ear infections can induce vomiting, along with dizziness (19). The symptoms here are similar to motion sickness, but in this case, the condition is caused by a bacterial or viral infection of the middle or inner ear. Labyrinthitis is one such inner ear infection that can lead to vomiting along with vertigo. Similar to motion sickness, the inner ear sends disoriented signals to the brain (due to infection), which in turn stimulates the abdominal muscles to contract and throw up.
Symptoms: Dizziness and imbalance, along with severe nausea and vomiting.
Treatment: After preliminary investigation, a doctor may prescribe steroids, antihistamines, antiemetics, or a vestibular suppressant to first address the symptoms caused by the infection. They may then prescribe antivirals or antibiotics to treat the infection itself (19).
13. Pneumonia
Pneumonia is an inflammation of the alveoli of the lungs due to bacterial or viral infection. A cough and trouble breathing are the major symptoms of this condition, but it can also manifest through vomiting (20). Vomiting and constant nausea are often triggered by a cough. It may also be triggered as a general effect of the infection since pneumonia leads to loss of appetite, which makes toddlers feel sick every time they eat something.
Symptoms: Vomiting is a less common symptom of pneumonia and is accompanied by more common symptoms such as a cough, cold, fever, and shortness of breath.
Treatment: A toddler with pneumonia may require a chest X-ray and blood tests to detect the extent of the inflammation and its cause. The toddler may be prescribed antibiotics to treat the underlying infection and paracetamol for fever and pain. Further, if the condition does not improve within two to four weeks or other symptoms develop, the toddler may be hospitalized and given intravenous medications along with fluids (20).
14. Certain infections and diseases
Vomiting is one of the several symptoms of infections, such as septicemiaiA severe blood infection, also called blood poisoning, caused when germs invade the body and meningitisiA bacterial or viral infection that can cause inflammation of the protective membranes that cover the brain and spinal cord (20). Dr. Hamid says, “After viral infections like rotavirus, some toddlers develop autoimmune gastritis, where the immune system attacks stomach cells. This can lead to chronic vomiting and nutrient deficiencies such as iron and B12 deficiency. Diagnosis requires anti-parietal cell antibody testing and endoscopic evaluation.”
Symptoms: Vomiting with a severe headache, body pain, fever, and cold shivers.
Treatment: A toddler may require blood tests, CT scan, and lumbar puncture along with physical examination to determine to which condition the symptoms match. Once determined, the child may be admitted to the hospital and given intravenous fluids and antibiotics to address dehydration and infection. They may also be provided with fresh oxygen and steroids for breathing difficulties and inflammations around the brain (22).
15. Rumination syndrome
Rumination syndrome is a rare and underdiagnosed condition in which an individual can regurgitate the contents of the stomach unconsciously, without any pain or trouble (23). Unlike the classic case of vomiting, rumination does not make the toddler feel uneasy or cause any discomfort or heartburn. It is a natural contraction of abdominal muscles to push the food upwards, which is beyond the control of the toddler.
This generally happens about 30 minutes after the last meal and does not create any secondary symptoms and problems. The expelled food tastes fresh, and the toddler will usually chew and swallow it back. It is a key trait that differentiates rumination from vomiting, in which case the expelled food is stale, semi-digested, and not fit to swallow.
There is no known cause for rumination, and it is speculated to occur due to problems in the nervous system. Since the cause is unknown and the condition rare, rumination syndrome is often misdiagnosed as some other reason for vomiting.
Treatment: Treatment of rumination syndrome is p Physiotherapy involving muscle training to promote the normal movement of abdominal muscles. The doctor may also prescribe some oral medication to subdue the involuntary urge of the nerves to stimulate regurgitation.
Considering the many causes of toddler vomiting but no fever, it is essential to know about the other symptoms associated with vomiting that warrant immediate medical attention.
When To See A Doctor?
Sometimes, your toddler’s vomiting could indicate a serious health ailment. One such instance is the case when the toddler is not able to hold any clear liquids in the body (24). Likewise, there are some other circumstances, when you should take your toddler to a doctor (25):
- There is blood in vomit: If the toddler is throwing up blood, then it could indicate a serious problem. They could be vomiting blood due to a severe stomach infection, bruised esophageal lining due to acid reflux, inflammation in the small intestine, and many other reasons. You must take your little one to a pediatrician as soon as possible.
- Vomiting is accompanied by high fever and acute diarrhea: As mentioned earlier, vomiting, accompanied by diarrhea, can dehydrate the child. If your toddler has a high fever, then it can make the condition even more distressful. A quick medical response is the best way to alleviate the condition.
- The vomit is always green or black: If the vomit is green, then it can be due to bile reflux, which could be an indicator of a serious intestinal infection or even ulcer. Black and dark brown vomit could be an indicator of blood clots due to internal bleeding previously. It can happen due to reasons ranging from milk allergies to deficiency of vitamin K.
- The abdomen is swollen: A visibly swollen tummy could be due to severe infection or fluid retention caused by a fundamental problem. Either way, it is an alarming sign and should be brought to swift medical attention.
- The toddler is fatigued and has a weakened pulse: These symptoms will be accompanied by decreased alertness and general disorientation. The toddler will urinate fewer times in the day, maybe once in eight hours. All these can be signs of severe dehydration due to loss of water and electrolytes through vomiting. The condition is aggravated if the toddler is also suffering from diarrhea.
- Stiff neck: If a child with vomiting has a stiff neck with or without photophobia (discomfort under bright lights), they should be provided immediate medical attention (26).
Vomiting could be spontaneous or acute, depending on the severity of the problem. When you are talking to your child’s doctor about vomiting, remember to mention:
- How often your child throws up and for how long.
- Describe the throw-up to your doctor. What color is it? Is it chunky or watery? Is there anything strange in it?
- Any accompanying symptoms including fever, diarrhea, stomach ache, or a swollen belly.
- How much your child is eating and drinking.
- How often your child pees and the color of the urine.
- If your child has recently eaten something new, taken a new medicine, or experienced anything new that resulted in throwing up.
- Has your child been acting differently and if they are more tired, grumpy, or less awake than usual.
Sharing your observations with the doctor can help them diagnose the issue and find the best treatment for your child.
Precautions To Prevent Vomiting
However, you can follow some generic safety measures to try and avoid the conditions that lead to vomiting (27).
- Always provide clean and hygienic food: Maintain cleanliness at home and in your kitchen. Clean the utensils you use for your toddler and sterilize them. Prepare your toddler’s food under hygienic conditions, as eating clean food is one way of preventing exposure to disease-causing bacteria and viruses.

- Limit the quantity of acid reflux and indigestion-causing foods: Foods such as chocolates, processed foods, and citrus fruits may cause acid reflux. If your toddler is prone to acid reflux, then limit the quantity of these foods. Also, ensure they eat slowly and not more than they need, to prevent overeating and digestive problems.
- Know the side effects of medicines before giving them to your toddler: Medicines may have side effects when consumed on an empty stomach. When giving your child such medicines, inquire from the doctor about all the probable effects on their digestion.
- Manage your toddler’s food allergy: If you know your toddler is allergic to a certain food, then prevent them from eating that food. Also, avoid the products that have the allergy-causing food as an ingredient.
- Avoid situations that may cause motion sickness: Do not take your motion-sick toddler for a ride on a mini-roller coaster in a theme park. Also, avoid other triggers like traveling through a long twisty road, a super-fast elevator, or anything that might make them throw up.
- Keep your child hydrated: Vomiting can dehydrate the body, and if it is accompanied by diarrhea, then it can quickly deplete the body’s water reserves. Keep a steady inflow of water and electrolytes to prevent the risk of severe dehydration in the case of vomiting. If you notice signs such as dry mouth, decreased urination, lethargy, and unusual irritability, seek medical attention immediately (28).
How To Make Your Toddler Feel Better?
If the precautions do not work, and your toddler is feeling sick, then you would want to make every effort to ease the condition. Here are some things you can do to make the child feel better:
- Do not force your little one to eat: Do not force your toddler to eat anything when they seem visibly distressed due to constant vomiting. It is okay if they skip a meal since they are doing so because of the discomfort caused by vomiting and the underlying problem. Even if they are hungry, give them liquids. Solid food may not be the right choice as their digestive system is not in a condition to digest it.
- Monitor your child’s eating habits: If your toddler consistently refuses to eat or drink, consult a healthcare provider promptly, as this could lead to rapid dehydration.
- Provide plenty of fluids: Feed them fluids since vomiting and diarrhea drain the body of water and electrolytes, such as sodium and potassium. Give your toddler fluids, such as dissolved oral rehydration solution/salts (ORS), in small sips or with a tablespoon. ORS is available in liquid or powder form over the counter and may be prepared by adding water according to the manufacturer’s instructions. ORS can also be made at home by mixing six leveled teaspoons of sugar and half a leveled teaspoon of salt dissolved in one liter of clean water. Do not mix ORS with formula or juice. This should rehydrate the child while giving them supplementary calories until they can eat solid food. Avoid giving milk and juices, as they can be difficult to digest (28) (29). The table below shows the minimum amount of liquid your child may need if they have dehydration.
| Child’s weight in pounds | Minimum amount of fluid to give per hour |
| 7 to 10 | 4 tablespoons or 1/4 cup |
| 11 to 15 | 5 tablespoons |
| 16 to 20 | 1/2 cup |
| 21 to 40 | 3/4 cup |
| 41 to 60 | 1 1/4 cups |
 Quick tip
Quick tip- Make your toddler rest: Ample rest helps the body in dealing with the infection that may have induced vomiting.

- Follow the prescribed course of medicines: The doctor will generally prescribe a course of treatment, which could involve multiple drugs. Follow the course without deviation to prevent a relapse of the infection.
What To Feed A Vomiting Toddler?
When the toddler vomits, the nutrients you have just tried to put into them are all gone. Moreover, they may simply refuse to eat after this unpleasant experience. In such a scenario, how will you make sure that they are getting enough energy? Follow these steps on feeding your toddler when they are vomiting (30):
- Stick to water and electrolytes initially: For hours after your little one last puked, give them small amounts of water and electrolyte solution. Do not attempt to feed them solid food any time soon since it can worsen the condition.
Dr. Chiriboga recommends, “In mild cases, provide extra hydration to the child. The best forms of hydration are plain water or an electrolyte solution. Avoid sugary beverages such as soda or juice. In severe cases, toddlers may need administration of an anti-emetic medication, either by mouth or injection.”
- Start with a liquid diet: Once your toddler seems better, you can start feeding them liquid food such as vegetable or chicken stock, with added salt and no added condiments. You can also give them rice stock but avoid lentil stock since certain lentils can be hard to digest. Tender coconut water works well, as it contains minerals and amino acids.
- Give bland solid food: Once they are fit enough to eat solid food, begin by giving them simple and bland foods. You can give them boiled and mashed rice with some vegetable or chicken stock. Boiled lentils and vegetables can be good, but stick to boiled vegetables, as they are easy to chew.
Do not give high fiber vegetables such as spinach and beans yet, since they are still recovering. You may blend and strain vegetables to make thin, easy-to-digest soups. You can put them back on a solid diet around eight hours after the little one last vomited.

- Once recovered, feed normally: If it has been 24 hours since the child vomited and they are responding well to the elementary diet, you can introduce them to solid foods. If your toddler consumes milk, you can reintroduce it along with other foods, such as plain bread. Start with small quantities of milk of not more than 100ml. Once everything seems fine, let your toddler have regular food that they are used to eating.
Remember, your toddler can speak a lot of basic phrases, therefore, they will let you know when they are hungry and want regular solid food. Do not force them to eat something or overwhelm them with food right after they have recovered. Giving some extra time for their body to get back on track will help prevent another round of vomiting.
Frequently Asked Questions
1. What is dry heaving in toddlers?
Retching, also referred to as dry heaving, is the act of dry vomiting when the abdominal and mouth muscles contract like they do in vomiting, but the toddler does not expel any substance from the mouth (31).
Toddlers dry heave after they have a bout of vomiting or when they are just feeling nauseated. The reasons for dry heaving are similar to vomiting, with the added cause that your toddler may also retch when he is feeling stressed or uncomfortable.
2. Is it normal for a toddler to have a fever while vomiting?
Vomiting, without any other accompanying symptoms, like fever, is not uncommon. Vomiting can happen for many reasons. As long as the toddler is active and has no fever or other accompanying symptoms, the chances are that the cause for vomiting is benign.
3. Why does my toddler throw up at night?
Handling a toddler throwing up at night can be quite challenging for parents, especially if it becomes a recurrent problem. Toddlers could throw up at night if they have skipped a meal, eaten just before bedtime, or eaten a large meal. In all these cases, the chances are that the digestive system has accumulated undigested food.
However, there could be other reasons too that could make a toddler throw up at night. A persistent cough is one of the reasons wherein toddlers could throw up at bedtime forcibly. This happens due to the gag reflex (32).
4. Do toddlers randomly throw up?
Yes. It is common for toddlers to throw up randomly. Indigestion, gastric reflux, and overfeeding are common reasons a toddler throws up occasionally. Occasional regurgitation is usually not a cause for concern. However, promptly speak to a doctor if the child’s vomiting frequency and intensity increase (1).
5. Should I let my toddler sleep after vomiting?
Yes. Your toddler should take adequate rest after a vomiting episode. Thus, if your toddler wants to sleep, let them sleep. However, ensure that they are well-hydrated. According to experts, sleep will help the stomach finish digesting food. It may also calm vomiting (33).
6. Can a toddler drink milk after vomiting?
It is not advisable to give milk or yogurt drinks until the vomiting has stopped for about eight hours (33).
7. How long does vomiting last in toddlers?
“The most common cause of vomiting in toddlers is a viral gastrointestinal illness, which may last for one to three days. Toddlers with persistent daily vomiting should consult their pediatrician to rule out any other underlying causes,” opines Dr. Chiriboga.
8. Is vomiting in babies and toddlers usually a common experience that will improve on its own?
Vomiting is a common symptom that babies and toddlers experience when they are sick (34). Once the cause is addressed it often gets better on its own. It is normal for them to vomit occasionally, but if it’s frequent or long-lasting, especially without a fever, it’s wise to see a doctor to rule out underlying causes like infections, food allergies, or gastrointestinal issues.
Vomiting in babies and toddlers is unpleasant but it is frequently a sign of a health problem and is accompanied by fever. However, don’t be alarmed if you notice that your toddler is vomiting but has no fever. Toddlers can vomit due to various reasons, including stomach and intestinal diseases, food allergies, and acid reflux. Treating the underlying condition will help your little one recover faster. In the meantime, ensure they drink plenty of water to avoid dehydration. If you notice any other serious symptoms in your toddler or frequent vomiting, visit a doctor promptly.
Infographic: Common Reasons For Vomiting In Toddlers
Several potential causes can induce vomiting in toddlers. To help you identify them, we have made a list that you can refer to. Also, ensure to keep your toddler hydrated by making them have enough fluids. If the vomiting persists or is accompanied by other symptoms, it is important to seek medical attention as early as possible.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Learn the best way to care for a child with vomiting and diarrhea. Get tips on how to keep them hydrated, what foods to avoid, and when to seek medical help.
References
- Diarrhoea And Vomiting In Children; NHS
https://www.cuh.nhs.uk/patient-information/diarrhoea-and-vomiting/” rel=”follow noopener noreferrer”> link2 - Bacterial Gastroenteritis; Cedars Sinai
https://www.cedars-sinai.org/health-library/diseases-and-conditions/b/bacterial-gastroenteritis.html - Appendicitis; Kids Health; Nemours
https://kidshealth.org/en/parents/appendicitis.html - Inguinal and Umbilical Hernias in Children; Stanford Children’s Health
ttps://www.stanfordchildrens.org/en/topic/default?id=inguinal-and-umbilical-hernia-90-P01998 - Types of Poisoning in Children; NYU Langone Hospitals
https://nyulangone.org/conditions/poisoning-in-children/types - Diagnosing Poisoning in Children; NYU Langone Hospitals
https://nyulangone.org/conditions/poisoning-in-children/diagnosis - Treatment for Poisoning in Children; NYU Langone Hospitals
https://nyulangone.org/conditions/poisoning-in-children/treatments/treatment-for-poisoning-in-children - Diagnosed Allergic Conditions in Children Aged 0–17 Years: United States, 2025; CDC
https://www.cdc.gov/nchs/products/databriefs/db459.htm#:~:text=4.4%25%20in%20children%20aged%200%E2%80%935%20years - Food Allergy; American College of Allergy, Asthma & Immunology
https://acaai.org/allergies/allergic-conditions/food/ - Food Allergies in Children; American Academy of Pediatrics
https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Food-Allergies-in-Children.aspx - Treatment -Lactose intolerance; NHS
https://www.nhs.uk/conditions/lactose-intolerance/ - Heartburn and GERD: Overview; National Center For Biotechnology Information
https://www.ncbi.nlm.nih.gov/books/NBK279254/ - Reflux in Children; National Institutes of Health
https://medlineplus.gov/refluxinchildren.html - Diarrhoea and vomiting; NHS
https://www.nhs.uk/conditions/diarrhoea-and-vomiting/ - By the way, doctor: What can I do about excessive belching and feeling full?; Harvard Medical School
https://www.health.harvard.edu/staying-healthy/what-can-i-do-about-excessive-belching-and-feeling-full - GERD (Gastroesophageal Reflux Disease) in Children; The Johns Hopkins University
https://www.hopkinsmedicine.org/health/conditions-and-diseases/gerd-gastroesophageal-reflux-disease-in-children - Indigestion; Nemours Children’s Health
https://kidshealth.org/en/parents/indigestion.html - Why Children Get Carsick—And What to Do; University of Rochester
https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=1&contentid=973 - Inner Ear Infection (Otitis Interna); Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/24240-inner-ear-infection-otitis-interna - Pneumonia; NHS
https://www.nhs.uk/conditions/pneumonia/ - Symptoms Checker for Toddlers; Meningitis Research Foundation
https://www.meningitis.org/meningitis/check-symptoms/toddlers - Treatment -Meningitis; NHS
https://www.nhs.uk/conditions/meningitis/treatment/ - Rumination Syndrome; University of Rochester
https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=134&ContentID=82 - Treating Vomiting; Healthy Children; American Academy of Pediatrics
https://www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/treating-vomiting.aspx - When To Take A Vomiting Child To The Doctor; University of Utah
https://healthcare.utah.edu/the-scope/kids-zone/all/2025/07/when-take-vomiting-child-doctor - Vomiting in children; Health Direct
https://www.healthdirect.gov.au/vomiting-in-children# - Nausea & Vomiting: Care and Treatment; Cleveland Clinic
https://my.clevelandclinic.org/health/symptoms/8106-nausea–vomiting - Dehydration: Giving Liquids at Home; Nationwide Children’s Hospital
https://www.nationwidechildrens.org/conditions/dehydration - Oral Rehydration Solutions; Made at Home: Rehydration Project
https://rehydrate.org/solutions/homemade.htm# - Should A Child Eat Or Drink If They Are Vomiting?; University of Utah
https://healthcare.utah.edu/the-scope/kids-zone/all/2025/08/should-child-eat-or-drink-if-theyre-vomiting - Mostafa Ebraheem Morra et al.; Definition of “persistent vomiting” in current medical literature; National Center for Biotechnology Information (2017)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5690699/ - My Child Coughs So Hard, they Vomit. Should I Worry?; University of Utah
https://healthcare.utah.edu/the-scope/kids-zone/all/2018/04/my-child-coughs-so-hard-they-vomit-should-i-worry - Vomiting; Nationwide Children’s Hospital
https://www.nationwidechildrens.org/conditions/vomiting - Vomiting; CHOP
https://www.chop.edu/conditions-diseases/vomiting
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Jenni Johnson
- Dr. Raashid Hamid is a consultant in the department of Pediatric Surgery at GMC hospital and associate professor of Pediatric and Neonatal Surgery at SKIMS, Jammu & Kashmir, India. He has four years of experience and specializes in general surgeries, including appendectomy, cholecystectomy, and exploratory laparotomy.
 Dr. Raashid Hamid is a consultant in the department of Pediatric Surgery at GMC hospital and associate professor of Pediatric and Neonatal Surgery at SKIMS, Jammu & Kashmir, India. He has four years of experience and specializes in general surgeries, including appendectomy, cholecystectomy, and exploratory laparotomy.
Dr. Raashid Hamid is a consultant in the department of Pediatric Surgery at GMC hospital and associate professor of Pediatric and Neonatal Surgery at SKIMS, Jammu & Kashmir, India. He has four years of experience and specializes in general surgeries, including appendectomy, cholecystectomy, and exploratory laparotomy. - Dr. Lauren Chiriboga did medicine at Florida International University Herbert Wertheim College of Medicine in Miami and a residency in pediatrics at Nicklaus Children’s Hospital. With over five years of experience as a pediatrician, Dr. Chiriboga currently works with Nicklaus Children’s Pediatric Care Centers.
 Dr. Lauren Chiriboga did medicine at Florida International University Herbert Wertheim College of Medicine in Miami and a residency in pediatrics at Nicklaus Children’s Hospital. With over five years of experience as a pediatrician, Dr. Chiriboga currently works with Nicklaus Children’s Pediatric Care Centers.
Dr. Lauren Chiriboga did medicine at Florida International University Herbert Wertheim College of Medicine in Miami and a residency in pediatrics at Nicklaus Children’s Hospital. With over five years of experience as a pediatrician, Dr. Chiriboga currently works with Nicklaus Children’s Pediatric Care Centers.
Read full bio of Rohit Garoo
Read full bio of Dr. Ritika Shah
Read full bio of Ghazia Shah