Image: Shutterstock
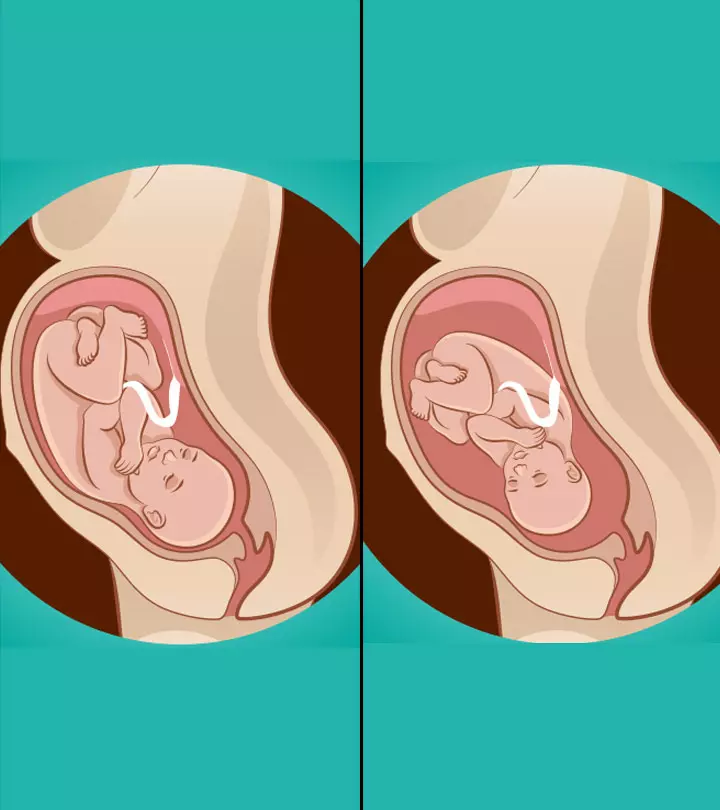
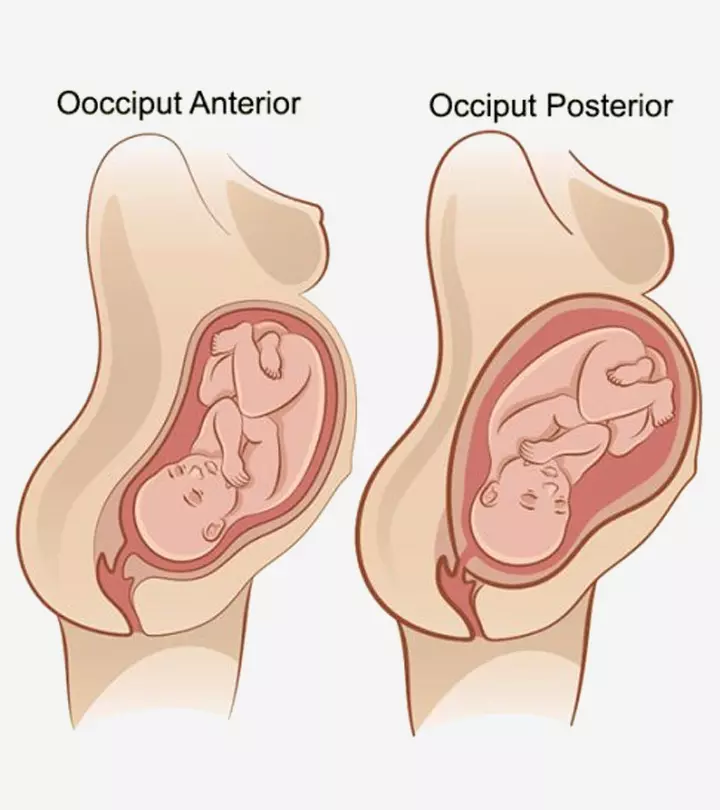
Occiput posterior position is when a baby is in vertex position (head-down) with their head facing to the front side of the mother in the womb. Babies can also be in various positions, such as head up, down, or facing back. Although it is safe to deliver vaginally in the occiput posterior position, it can be harder for babies to pass through the birth canal. In addition, some babies may turn to other positions before delivery.
Read on to learn more about the occiput posterior position, its causes, and what complications may arise during labor.
bies in the OP position usually need assisted
Key Pointers
- Occiput posterior (OP) refers to a head-down position of the baby facing the front of the mother’s womb.
- Some risks associated with OP include postpartum hemorrhage, perineal tears caused by forceps or vacuum, and prolonged pre-labor.
- C-sections, forceps, and vacuums may be utilized to aid in the delivery of an OP baby.
- The shape of the pelvis, curvature of the spinal cord, age, ethnicity, weight, and previous OP births may all contribute to the occurrence of OP.
- Preventative measures for OP include improving body posture, engaging in exercises, consulting chiropractors and acupuncture therapists.
What Does Occiput Posterior Position Mean?
A head-down position of the baby facing your abdomen (and not the back) is called an occiput posterior (OP) position.
The vertex presentation wherein the occiput (back of the baby’s head) is anteriorly (to the front) positioned is called occiput anterior and is considered one of the optimal baby birth positions for childbirth (1).
There are two OP positions:
Right occiput posterior: ROP has the baby’s back facing towards the right side of the mother and the back of the head facing towards the mother’s back.
Left occiput posterior: LOP has the baby’s back facing the left side of the mother and back of the head towards the mother’s back (1).
The baby could also be in a straight OP position:
OP occurs due to certain physical and lifestyle reasons.
 Quick fact
Quick factCan An OP Position Affect Labor?
Here is what could happen in the case of posterior labor:
- Most babies, who are in the occiput posterior position before labor, tend to rotate to the occiput anterior (OA) position after the labor sets in.
Haley Callahan, a mom and doula, shares about her baby’s position during the 32nd week of pregnancy. She writes, “At our midwife appointment on Tuesday, the little one was perfectly sized and in the occiput posterior position, meaning he/she is head down with his/her legs facing outward. We’ve still got lots of time – and the baby’s probably already in another position – but eventually, we want the baby to flip around so that his/her legs are facing my spine for the birth (i).”
- Some posterior babies may get delivered without any slowdown in labor, while some may take time but require no obstetric interventions.
- When the posterior baby might not turn, or the possibility of vaginal delivery is low, then the mother may have to undergo a C-section.
- Deliveries with babies in the OP position usually need assisted methods such as a C-section or the use of vacuum and forceps.
In some cases, the babies may not turn and could make the labor difficult (2).
What Could Be The Complications Of A Posterior Labor?
Here are the possible complications for the mother and the baby in the case of posterior labor (3) (4):
- Possible risk of postpartum hemorrhage (more than 500ml of blood loss), and infections
- Delivery done using forceps and vacuum may cause third and fourth-degree perineal tearsiA vaginal pull or minor injury that is common during normal delivery , particularly if the mother has insufficient cervical dilation.
- A longer lasting pre-labor (first and second stage), with a backache
- Needs frequent induction to start the labor, and its failure may necessitate a C section.
- Chorioamnionitis, also called intra-amniotic infection (IAI), is the inflammation of the fetal membraneiProtective layer of tissues surrounding the fetus during pregnancy due to bacterial infection
According to the Eunice Kennedy Shriver National Institute of Child Health and Human Development, clinical chorioamnionitis affected 15% of pregnant women during the antepartum period (the period before childbirth), while the others 85% were affected during the intrapartum period (the period from onset of labor to delivery).
- A baby delivered in the OP position might have chances of a low APGAR scoreiA scoring system used to assess the health status of newborns within a few minutes after birth (less than 7), meconium-stained amniotic fluidiPresence of meconium (first newborn stool) in the amniotic fluid , meconium aspirationiA medical condition in which newborns inhale amniotic fluid and meconium (their first stool) during the birthing process birth trauma, NICU admissions, and longer neonatal stay (5)
- This fetal position might also increase the risk of birth-related complications such as umbilical cord prolapse.
These complications could make labor difficult in OP cases, affecting maternal and neonatal health. Some women are likely to have a tougher time than others.
Posterior labor is likely to be less difficult if:
- The baby is smaller or average in size
- The posterior baby engages during labor.
 Point to consider
Point to considerYour OB/GYN would do everything possible to manage the OP position and avoid any complications.
What Causes A Baby To Get Into Occiput Position?
Some factors that could lead to an occiput posterior baby are (6):
- The shape of the pelvis: Anthropoid and android-shaped pelvises could lead to OP. Women with a heart-shaped pelvis (android) may have the baby in this position because of the narrower front.
A pelvis with an oval-shaped inlet, with a large anterior-posterior diameter (anthropoid) and a narrow pelvic cavity, may also lead to OP.
- Maternal kyphosis: The mother’s kyphosis or hunchback (excessive curvature of the spinal cord) could make the fetal back fit into the curve. Multiple pregnancies (twins or more) may also be a reason for this position.
According to the Centers for Disease Control and Prevention, the twin birth rate is 31.2 per 1,000 live births while the rate of three or more births is 80.0 per 100,000 live births in the United States.
These causes might increase the chances of OP during delivery if you belong to the high-risk group.
The Risk Factors That Might Increase The Chances Of OP
Here are the factors that may influence your chances of having an OP position during the delivery (7).
- Your age is more than 35 years
- Nulliparity – you haven’t given birth before
- Previous OP delivery
- Obesity
- Decreased pelvic outlet capacity
- African-American ethnicity
- Birth weight of more than 4,000g
- Gestational age of more than 41 weeks
An OP position might complicate the labor by prolonging it. Timely diagnosis and management could help minimize the implications.
Diagnosis And Management Of Occiput Posterior Position
The OP position could be diagnosed through an ultrasound scanning, and its management is done only if the fetal heart rate is reassuring.
An OP may be managed through:
- Operative vaginal delivery
- C-section
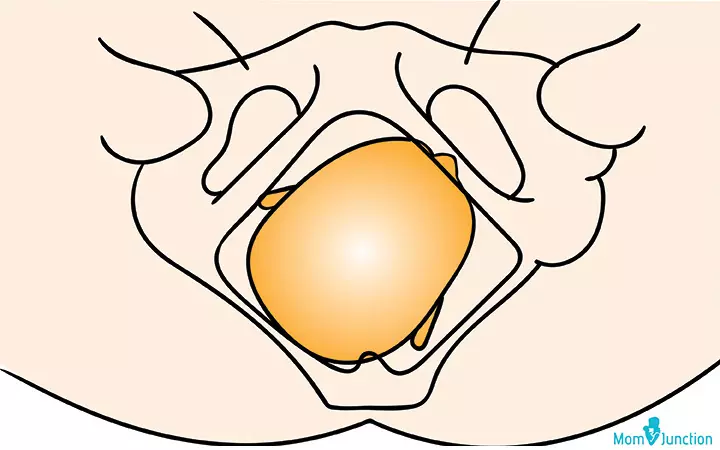
Operative vaginal delivery from the OP position: It could be done if there is sufficient room between the occiput and the sacrumiFlat triangular shaped bone located near the base of the spine that connects with the pelvis , allowing the baby to turn. Forceps or a vacuum extractor may be used to bring the baby out (8).
C-section: This is done when the positioning techniques do not help you deliver the baby through the vagina.
Occiput posterior may not be as serious as a breech position, but it is not as easy as the occiput anterior either. Therefore, you may try preventing OP and get the baby to the easier OA position (13).
Other management techniques for an OP position include maternal positioning and manual fetal rotation. However, their effectiveness may vary based on the mother’s health, the healthcare team’s skill, and the potential risks involved
 Did you know?
Did you know?How To Prevent An Occiput Posterior Position?
Following the below postures and exercises might help keep the fetus in an appropriate position and facilitate delivery (9).
- Postures: Avoid reclining positions and sit with your pelvis tilted. You could use a birth ball to maintain this posture. Sleep towards the left side, keeping left leg straight and right leg at 90 degrees, supported with pillows between the legs.
- Exercises: You may perform exercises that involve pelvic rocking, walking, and swimming. Here is what you could do:
i. During pre-labor: Pelvic rocking for ten times for 2-5 times a day is likely to help in rotating the hips in a circular motion. Get down on your hands and knees, and lean forward as much as you can comfortably. Repeat this during the early stages of labor; it could help ease back and pelvic pain.

Image: Shutterstock
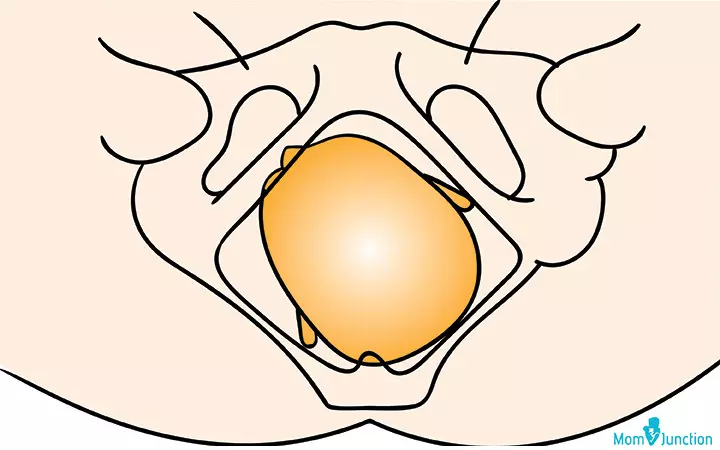
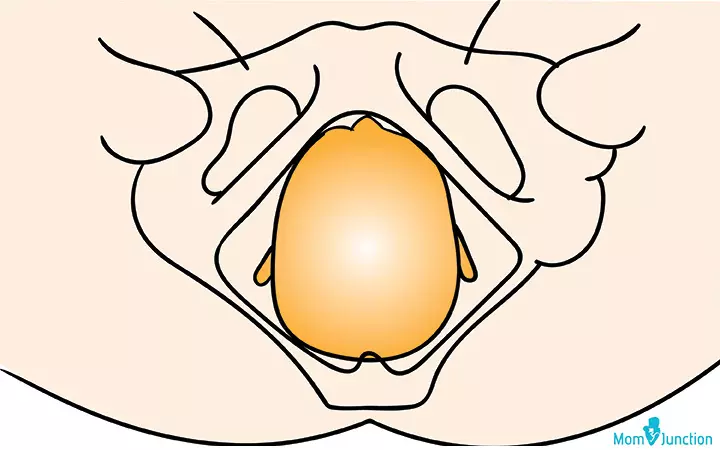
ii. Towards the end of the first stage of labor: If the baby is moving towards an OA position, then squatting could help relax the pelvic floor muscles, creating more room for the baby to rotate.

Image: Shutterstock
iii. During the pushing stage: Doing double hip squeeze during the contractions may help the pelvis spread, providing more room for the baby to move back to the right position.
- Therapies: Chiropractic and acupuncture techniques may help fix the improper alignment of your body and turn the baby to the OA position.
Note: Ensure that the exercises and therapies that you consider are approved by your doctor.
Frequently Asked Questions
1. How to deal with posterior labor pain?
During posterior labor, the process may get prolonged, making you feel tired. In such a case, you may want to go for an epiduraliInjection with anesthetic property, administered to alleviate pain during labor to get relief from the pain. However, an epidural anesthesia might decrease the chances of your baby’s rotation to the anterior position. This, in turn, could prolong the second stage of labor or increase the chances of forceps delivery.
- You may also try breathing techniques.
- Try to lean forward during the labor as it helps in relieving the back pain to some extent.
- Use a hot or cold compress.
- Get your lower back massaged.
2. If my baby is posterior during labor, does that mean I’ll have back labor?
It is not necessary, but there could be a high chance. A study has found that one in four women experienced back labor, but not all of them had a posterior baby (10).
3. What is the OP C-section rate?
Around 18% of the OP cases were found to result in emergency C-section or assisted delivery in a randomized controlled study (4).
4. What percentage of babies are occiput posterior?
According to various studies, about 10-34% of fetuses are presented in an occiput-posterior (OP) position during the first stage of labor (13).
5. Can I give birth if the baby is in the occiput posterior position?
Although most cases of fetuses in occiput-posterior (OP) position change their position when in labor if the position is not changed, a woman can still give vaginal birth to a baby (14).
Occiput Posterior Position is when the baby lies in a head-down position facing the mother’s abdomen before birth. It may prolong the labor and delivery process requiring medical assistance such as a C-section, vacuum, and forceps. In addition, posterior labor may increase the risk of postpartum hemorrhage, and intraamniotic infection for the mother and the baby may require longer neonatal care. Factors such as advanced maternal age, nulliparity, obesity, longer gestation may increase the risk of having an OP position. It may be prevented by maintaining good posture, chiropractic treatment, and other alternative therapies.
Infographic: Consequences Of Manual Rotation For Persistent Occiput Posterior Position
Manual rotation for persistent occiput posterior position may help to change the fetal presentation in some cases. Although there are a few benefits, they can be associated with various risks. The procedure is often considered in cases of expected positive outcomes. Check the infographic to know the outcomes of manual rotation during labor. Illustration: Momjunction Design Team
Wondering what are the complications associated with Occiput posterior? Watch this video to learn about the mechanism of occiput posterior labor and how it can be managed with long rotation.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Healthy + Hapai–32 WEEKS;https://greenplatedinners.wordpress.com/category/pregnancy/page/6/
References
1. Fetal Position; OB-GYN 101: Introductory Obstetrics & Gynecology; Medical Education Division, Brookside Associates, Ltd.
2. Delivery presentations; U.S. Department of Health and Human Services National Institutes of Health (2019)
3. Senécal J et al.; Effect of fetal position on second-stage duration and labor outcome; Obstet Gynecol (2005)
4. Hala Phipps et al.; Persistent Occiput Posterior position – OUTcomes following manual rotation (POP-OUT): study protocol for a randomised controlled trial; Trials (2015)
5. Cheng YW et al.; The association between persistent occiput posterior position and neonatal outcomes; Obstet Gynecol (2006)
6. Diaa M. EI-Mowafi; Malposition and Malpresentations; Geneva Foundation for Medical Education and Research (2019)
7. Cheng YW et al.; Associated factors and outcomes of persistent occiput posterior position: A retrospective cohort study from 1976 to 2001; Birth (2010)
8. Pearl M et al.; Vaginal delivery from the persistent occiput posterior position. Influence on maternal and neonatal morbidity; J Reprod Med (1993)
9. Posterior Babies; The Midwifery Group, Vancouver
10. Back Labor; Women’s Birth & Wellness Center, North Carolina
11. Marie Biancuzzo; How to Recognize and Rotate an Occiput Posterior Fetus; The American Journal of Nursing (1993)
12. Getting your baby into the best birth position; Tommy’s
13. Marie-Julia Guittier et al.; Maternal positioning to correct occipito-posterior fetal position in labour: a randomised controlled trial; BMC Pregnancy and Childbirth (2014)
14. If your baby is posterior when you are in labour; Midwifery Led Unit; Cavan General Hospital
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sangeeta Agrawal
Read full bio of Sakshi Mishra
Read full bio of Rebecca Malachi
Read full bio of Aneesha Amonz