Image: Shutterstock
The process of giving birth is painful. One widely used method that helps relieve pain in women is epidural analgesia for labor. According to the American Pregnancy Association, more than 50 percent of women who opt for hospital birth use epidural anesthesia. Most women choose this technique to cope with the pain during labor and childbirth. If you are a first-time mom, you may be wondering about the safety, efficacy, and other aspects of this medication. Reading this post may help you explore the contents, benefits, side effects, and more on administering epidural during labor.

Key Pointers
- Epidural analgesia is a pain-relieving treatment used during labor and childbirth.
- The treatment involves injecting a mixture of local anesthetics and opioids into the epidural region of the spine.
- Epidurals offer several benefits, including excellent pain management and facilitating the baby’s movement during birth.
- However, an epidural can also cause adverse effects such as a drop in blood pressure, nausea, headaches, and dizziness.
- To ensure the safety of the baby, doctors continuously monitor the fetal heart rate during labor and may also administer synthetic oxytocin to induce contractions.
What Is An Epidural?
Epidural analgesia is local anesthetic injected into the epidural space of the spine, to numb the spinal nerves and offer relief from the pain during labor
(1). The drug travels through the epidural space to the nerves and works by stopping the pain signals from reaching the brain. Choosing the right anesthetic technique can help manage pain during labor and reduce the risk of anesthesia complications.
Since it is injected into the lumbar region of the spine, pregnant women do not feel any sensation in the lower half of the body. For women who do not want to experience natural labor pain and do not want to take medications, epidural analgesia has become the choice of labor pain relief.
Note that an epidural is not the medicine itself, but a procedure of administering anesthetics for pain management.
Drugs In An Epidural
Epidural medications are a combination of local anestheticsiMedications used during the surgeries and tests to cause numbness. (bupivacaine, levobupivacaine, or ropivacaine) and opioidsiA category of painkillers that interact with opioid receptors in the body to relieve pain. (fentanyl, diamorphine, morphine, and sufentanil). The opioid dosage used in epidural is (2):
| Opioid | Epidural |
|---|---|
| Sufentanil | 25-50µg |
| Fentanyl | 50-100µg |
| Diamorphine | 2.0-3.0mg |
| Morphine | 7.5-10mg |
Local anestheticsiMedications used during the surgeries and tests to cause numbness. lidocaine and chloroprocaine are not used nowadays because the action time for chloroprocaine is too short and repeated doses of lidocaine are found to cause tachyphylaxisiReduced response of the body to a drug after repeated exposure or administration.
.
When administered the right way, these epidural combinations can be highly effective and beneficial for managing pain during delivery.
What Are The Benefits Of Epidurals?

Image: Shutterstock
Epidurals (3):
- Are more effective than other pain-relief options during labor.
- Make movement easy and give you the strength to push out your baby.
- Can be administered at any stage of labor.
- Are very safe in experts’ hands.
- Help you stay awake and alert during delivery (4).
- Can be used to numb only the lower part of the body in case of a C-section.
- Help you get rest and stay focused, especially if you feel exhausted.
Elissa Levy, a mother of two, shares how epidural helped her have a positive birthing experience. She says, “Those contractions were horrible… The epidural needle hurt WAY less than last time, and the epidural worked like magic. I was comfortable for a while. The nurses kept asking if I needed anything, and I was like, “Nope, I’ll never need anything again, as long as I have this epidural.” They said when I feel pressure when I feel like it’s time to start pushing, they’ll call the doctor. Then I started to feel my contractions more strongly despite the epidural, though it was still much more tolerable than before the epidural. The nurse said I can keep my epidural strength (or even ask for more, which I didn’t) as long as I could feel my contractions in order to be ready to push… Finally, the doctor came back and said I could push (i).”
Besides the benefits, you should also know about the exact procedure of epidural analgesia before opting for it.
 Quick fact
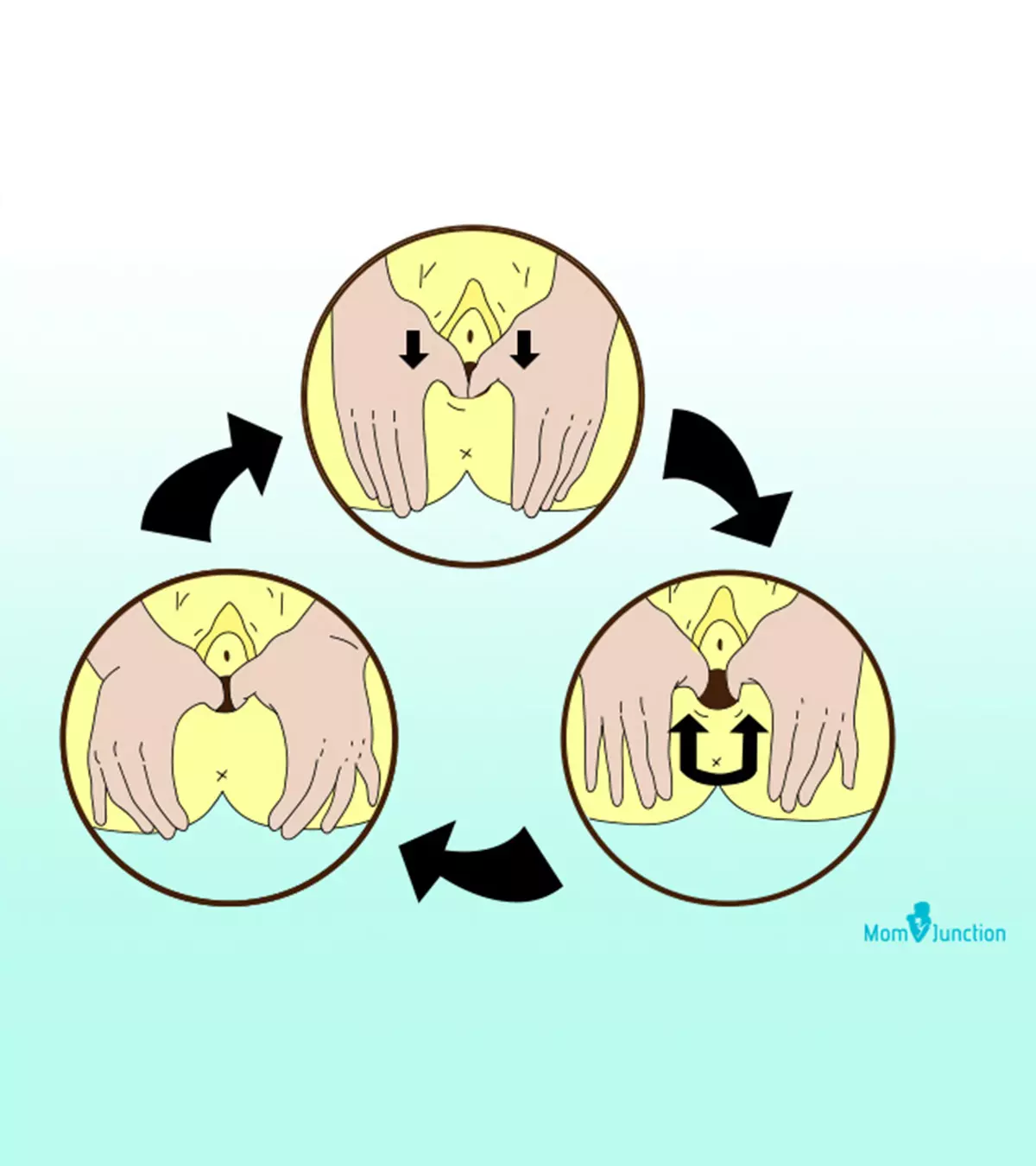
Quick factHow Is An Epidural Administered?
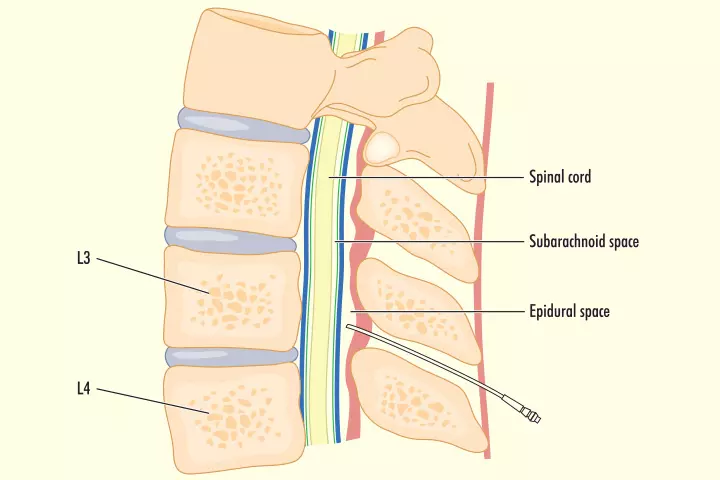
Image: Shutterstock
An anesthetist administers the epidural. The procedure is explained next, in detailed steps (5):
- Before giving you the anesthesia, the doctor will insert a drip into your arm.
- You will be asked to sit upright straight or lie on your side with the back curving towards the anesthetist. A nurse can help you to get into the desired position.
- The specialist will apply a cold, antiseptic solution to the area of the skin where he injects the local anesthetic.
- You have to stay still and not move when the doctor puts the epidural in. The doctor may ask you to report any contractions at this time.
- A needle with a catheter containing the epidural medication will be inserted into the epidural space of the spine. The needle will be removed, and the catheter stays put in that place, secured with a bandage, until after delivery.
- 15 minutes after epidural administration, you will feel the pain subside.
- You will be able to move around or on the bed comfortably, with the catheter attached at the back. However, you should not slide or drag the lower back as it can pull off the catheter.
- If the initial dose does not work well, then the midwife can give you more medication.
Once the epidural is given, the doctor will monitor the fetal heart rate continuously during the labor. A CTG machineiA cardiotocograph machine used to monitor fetal heart rate and uterine contractions. is used to measure the fetal heart rate and your contractions.
Doctors may give you synthetic oxytocin (Pitocin) to induce contractions.
Though epidural analgesia reduces pain during delivery, it can have some side-effects.
Side-effects Of Epidural
Epidurals are generally safe, but there are some side-effects (6).
- Epidurals can lengthen the second stage of labor.
- They can cause a drop in the blood pressure, making you dizzy and nauseated. In the case of a sudden blood pressure drop, IV fluids, oxygen, and medication may be given to you.

Image: IStock
- Around 23 out of 100 women get a fever due to the epidural (7).
- Loss of excess spinal fluid, if the needle is inserted accidentally in the subarachnoid spaceiThe space containing cerebrospinal fluid (CSF), main blood arteries, and cisterns (fluid-filled spaces). , can result in a headache.
- You can feel weakness in the leg muscles.
- Numbness in the lower body makes it difficult for you to sense the urge for urination. Thus a urinary catheter needs to be inserted. 15 out of 100 women face this problem.
- The chances of vaginal delivery reduce to some extent.
- Reduced muscle strength and the inability to push effectively during labor can lead to assisted or instrumental delivery using forceps and vacuum extraction. Around 14 out of 100 women who have an epidural have an assisted delivery (7).
- An assisted delivery requires an episiotomy (a cut in the back of vagina) that needs stitches.
- Stopping the epidural in the later stage of labor can result in more pain and doesn’t make birthing easier.
- Epidurals can cause itching, which can be treated with antihistaminesiMedications that relieve allergic symptoms. .
- You may experience pain or tenderness in the injected area.

Image: Shutterstock
- Slow breathing or drowsiness can be a side effect.
- The epidural catheter can cause temporary damage to the nerve.
- Permanent nerve damage that can cause loss of movement or sensation in one or both legs, although rare, can be a major side-effect (8).
- A bruised feeling and possible infection around the skin where the catheter is inserted.
If the epidural analgesia fails to block the pain entirely, the procedure might be repeated, or you will be offered an alternative method of pain relief (9).
Some alternative methods of pain relief utilized by surgeons during childbirth or an obstetric surgery may include regional anesthesia and neuraxial anesthesia. However, a pain relief technique is chosen after considering the patient’s safety and minimizing the risks of the chosen method.
While it is uncommon, there may be instances of anesthesia complications during labor. However, the risk of such complications can be minimized by using suitable pain control measures and ensuring careful monitoring.
Very rare complications of an epidural include:
- fits (convulsions)
- severe breathing difficulties
- death
 Did you know?
Did you know?Alternatives To Epidural
Expectant mothers who choose not to use epidural anesthesia for pain relief may opt for alternative birthing methods, which may include (10) (11):
- Breathing and relaxation techniques
- Hypnosis or hypnobirthing (may include visualization, relaxation, and deep breathing techniques)
- Birthing ball
- Water birthing
- Using TENS (transcutaneous electrical nerve stimulation) technique
Natural Birth Vs Epidural
Natural childbirth typically does not involve any medical interventions such as pain medications, epidurals, or continuous fetal monitoring. It is suitable for low-risk pregnancies and offers the benefits of avoiding the side effects of medicines, such as nausea, altered speed of labor, and hypotension. However, it is not advisable for high-risk pregnancies (10). On the other hand, an epidural could be administered for medical reasons during the childbirth process, and it provides effective pain relief for the mother. However, as mentioned above, it has a risk of certain side effects. Ultimately, the choice between a natural birth and an epidural birth significantly relies on pain tolerance levels, medical factors, and personal preferences of the mother, and it is essential to talk to your healthcare providers to make an informed decision considering your health circumstances.
If you are considering an epidural but still have doubts about it, keep reading to get the answers.
Frequently Asked Questions
1. Do epidurals increase the chances of a C-section?
There is no proof that epidurals increase the likelihood of a C-section. If you have doubts, talk to your doctor about it (5).
2. Who should not get an epidural?
Avoid epidurals in case of:
- Blood clotting disorders
- Use of medications for blood thinning
- Neurologic disorders
- Heavy vaginal bleeding
Epidurals are also not ideal for women who have had lower back surgery.
3. How long does it take to inject an epidural?
The procedure lasts around ten minutes, and the pain starts to subside five minutes after administration. However, the time taken for the procedure may exceed in case of obese women or women with abnormal spine.
4. When will the epidural be administered?
An epidural is administered during active labor or on the demand of the patient or based on the circumstances, the doctor usually decides the best time to inject an epidural.
5. Do I need an epidural during labor?
If you can cope with labor pain easily, there is no need of taking an epidural injection. It will be given only upon your request.
6. Will the epidural injection hurt?
7. Does epidural have any effect on the fetus?
Epidural analgesia enters the mother’s bloodstream and reaches the fetus through the umbilical cord and doesn’t have any strong impact on the baby’s health. However, it might prevent the baby from attaining the best position, leading to assisted vaginal delivery. According to a study, 10 out of 100 women need an instrumental delivery without having an epidural and 14 out of 100 women need it with an epidural (7).
8. Does epidural always work?
In the majority of cases, epidural brings adequate relief from labor pain. However, there are cases when the epidural does not work effectively. This could be due to improper insertion of the catheter in the epidural space, owing to the problematic neuraxial anatomy of the patient. This hastens the labor process or can prevent the epidural block from acting on time (12).
9. How far dilated is too late for an epidural?
An epidural is usually not given until the cervix is at least three to four centimeters dilated. An epidural is considered too late when the mother is fully dilated (13).
10. How long does back pain last after an epidural?
Some women may experience lower back pain that may last for a few hours to a few days after an epidural (14).
Several mothers opt for epidural analgesia to relieve pain during labor. Epidural is the most effective pain-relieving option that can be administered at any stage of labor. It keeps you alert and awake during labor and gives strength to push out your baby. Generally, epidural analgesia during labor is safe. However, it can have mild side effects. Besides, it isn’t a suitable option in cases where an expecting mother is on blood-thinning medications or had lower back surgery. As you near your due date, discuss different pain-relieving options with the doctor and make an informed choice.
Infographic: Epidural Analgesia Administration Procedure To Counter Labor Pain
One of the most challenging parts of pregnancy and childbirth is labor pain. However, epidural analgesia, a local anesthetic approach, helps relieve labor pain. In the below infographic, we present the procedure of epidural administration and what happens after that, helping you make informed decisions related to this procedure.
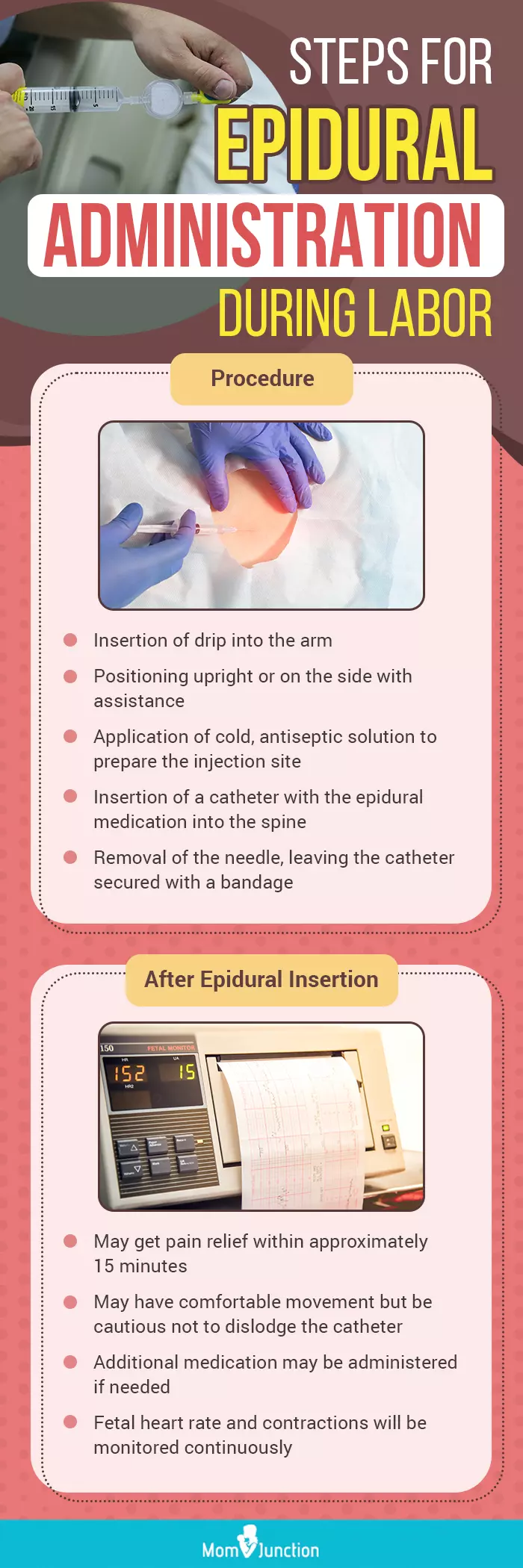
Illustration: Momjunction Design Team
Whether it is your first birth or you’re experiencing slow labor progression, your doctor may advise you for epidural analgesia to safely and effectively manage labor pain. Watch this video to learn more about this procedure.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Back to the delivery room.https://elissa-dunn-levy.medium.com/back-to-the-delivery-room-95da68e9ef2a
References
- Epidural and Spinal Anesthesia.
https://www.uofmhealth.org/health-library/rt1583 - Elizabeth McGrady and Kerry Litchfield; (2004); Epidural analgesia in labour.
https://academic.oup.com/bjaed/article/4/4/114/308005 - Adrian N. Avila Hernandez; Paramvir Singh; Epidural Anesthesia.
https://www.ncbi.nlm.nih.gov/books/NBK542219/ - Epidurals.
https://madeforthismoment.asahq.org/pain-management/techniques/epidural/ - Childbirth.
https://www.med.unc.edu/anesthesiology/patients/childbirth-1 - Childbirth – pain relief options.
https://www.betterhealth.vic.gov.au/health/healthyliving/childbirth-pain-relief-options - Pregnancy and birth: Epidurals and painkillers for labor pain relief.
https://www.ncbi.nlm.nih.gov/books/NBK279567/ - Nerve damage associated with a spinal or epidural injection.
https://www.esht.nhs.uk/wp-content/uploads/2017/06/0191.pdf - Side effects – Epidural.
https://www.nhs.uk/conditions/epidural/side-effects/ - Natural Childbirth.
https://kidshealth.org/en/parents/natural-childbirth.html - Pain relief in labour and birth.
https://www.tommys.org/pregnancy-information/giving-birth/pain-relief - Katherine Arendt and Scott Segal; (2008); Why Epidurals Do Not Always Work.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2505163/ - Epidural Pros and Cons.
https://www.birthinjuryhelpcenter.org/birth-injuries/help-center/epidural/ - Laboring under misconceptions: Epidural myths may keep women from reliable pain management.
https://www.asahq.org/about-asa/newsroom/news-releases/2014/06/epidural-myth - Epidural.
https://my.clevelandclinic.org/health/treatments/21896-epidural#risks–benefits
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Suman Lal
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das