
Image: Shutterstock
Breastfeeding is one of the most rewarding aspects of motherhood and has several benefits for the mother and baby. However, it is not free from its share of challenges. Some breastfeeding complications, such as mastitis, can make this experience uncomfortable and painful and even make some moms hesitant to breastfeed.
Read on to learn more about mastitis, including its causes and treatment options, as well as prevention suggestions.
What Is Mastitis?
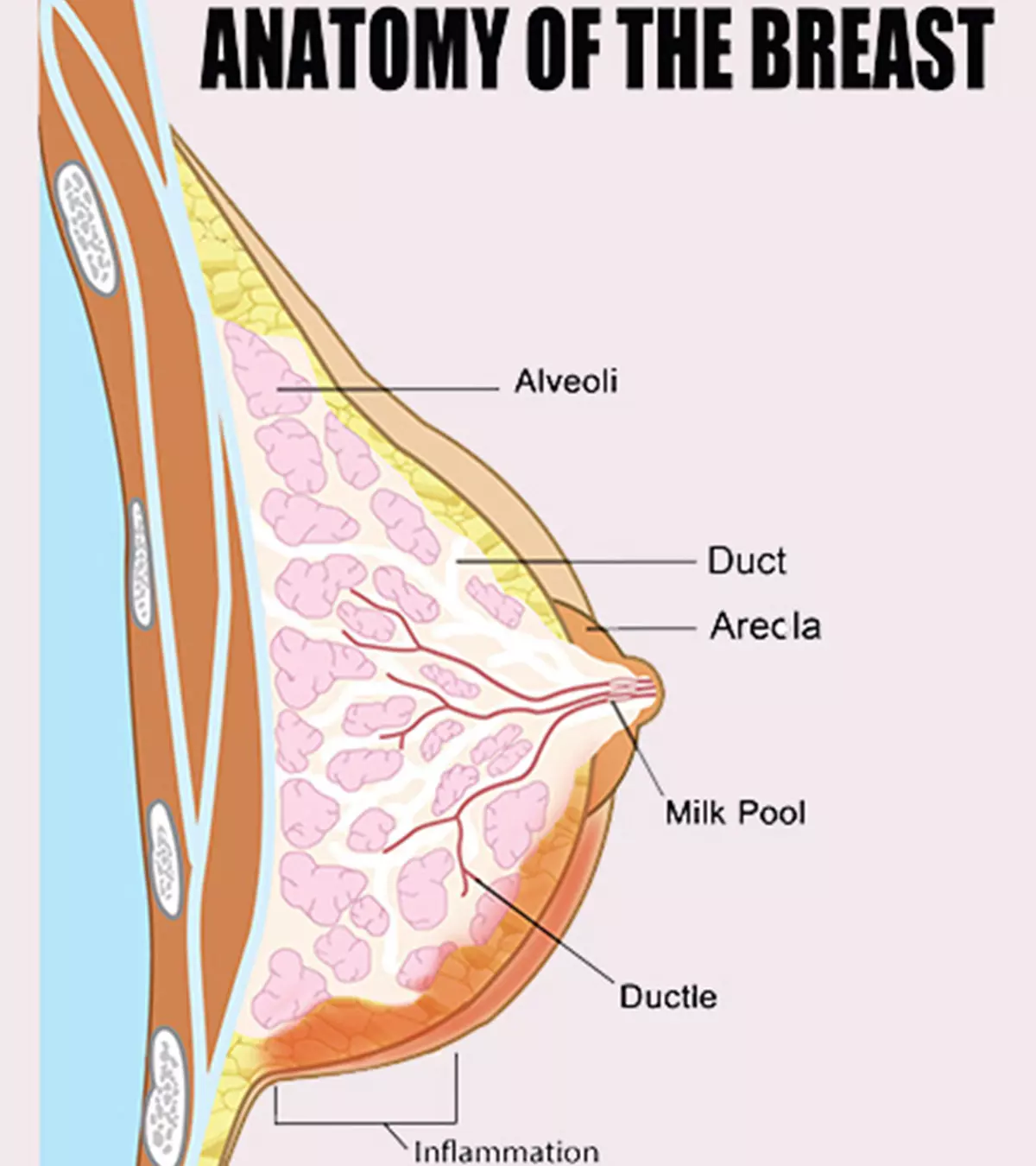
Mastitis is the engorgement of the breasts due to the accumulation of milk in them. This leads to bacterial infection of the milk ducts (1) and results in infective mastitis.
Mastitis can be lactation mastitis, also called puerperal mastitis, which happens among breastfeeding women. It occurs due to the retention of milk in the breasts for far too long.
Another type is periductal mastitis, which occurs in non-breastfeeding women. Periductal mastitis is the inflammation of the breast, caused by bacteria entering the breasts through a cracked or sore nipple.
In this article, we primarily focus on lactation mastitis. Lactation mastitis is most concerning for women since it affects their ability to breastfeed. Interference with breastfeeding has an impact on the nourishment of the baby.
How Common Is Mastitis?
About 10% of breastfeeding mothers develop mastitis, usually during the first six months of lactation (2). The risk is the highest during the first three months after delivery when you’re feeding a newborn. That said, the risk is there for as long as you are breastfeeding.
What Causes Mastitis?
The primary cause of mastitis among breastfeeding mothers is milk stasis, a condition where milk is retained within the breast long enough to block milk ducts (3). When that happens, milk from the ducts may spill over to the surrounding tissue, triggering an autoimmune response. The immune system detects milk protein as a bacterial or viral protein and mounts an inflammatory reaction, causing swelling.
Bacteria such as the Staphylococcus and Streptococcus can slip inside a sore or cracked nipple and infect the milk duct. E.coli, Mycobacterium and the fungus Candida (Yeast) are other pathogens that can also lead to infections.
But what causes milk retention in the breasts? Keep reading to know.
- The baby is not latching correctly to the breast: When the baby is unable to latch properly to the breast, he or she may not be able to feed properly or get the required nourishment, causing milk retention in the breasts. Poor latching could be due to conditions such as a cleft lip or tongue-tie in the baby, or because the mother is unable to get her baby to latch correctly.
- Missing feeds too often: If you miss feeding the baby often, then your milk does not drain as and when it should.
- Favoring one breast: You or your baby may prefer one breast to the other, leaving the latter full. Retention of milk for too long can cause milk stasis and eventually mastitis.
- Weaning quickly: If you wean your baby too fast, then your breast may not have a way to drain the milk it is producing, causing milk stasis.
- Pressure on the breast: An improperly fitting bra or a tight dress can create unnecessary stress on the breast tissue, narrowing the milk ducts. Narrowed milk ducts are harder to drain during suckling and lead to milk retention.
- Injury to the breast: A severe blow or impact to the breast may rupture a milk duct, causing inflammation and infection, and make breastfeeding difficult.
Some women are more prone to the problem than others. Let’s see why.
What Are The Risk Factors For Mastitis?
The following conditions or lifestyle choices increase the risk of lactation mastitis (2):
- Previous bacterial mastitis infection. If you already suffered a bout of mastitis, then you could be at a higher risk of getting infected again.
- Using plastic breast pads can prevent adequate air circulation and ventilation, and make the breasts susceptible to infection.
- Poor maternal nutrition and maternal deficiencies such as anemia reduce the body’s ability to fight infections.
- Piercings cause a crack in the nipple, allowing bacteria to enter the milk ducts.
- The baby has strep throat or thrush (yeast infection) while you have a cracked nipple. The pathogen may enter the breast, causing mastitis.
- Smoking seems to increase the chances of developing mastitis (4).
What Are The Symptoms Of Mastitis?
The symptoms of mastitis are:
- Engorgement and inflammation of the breast.
- Redness of the breast. The reddened regions also feel hot when touched.
- The affected part of the breast feels hard when touched.
- Acute pain and tenderness of breasts.
- Burning sensation while breastfeeding.
- White or yellowish discharge from the nipple.
- Flu-like symptoms including body aches, fatigue, and a fever of 100.4°F (38°C).
If you notice any of the symptoms, visit a doctor at the earliest.
How Is Mastitis Diagnosed?
Your doctor will diagnose mastitis through the following procedures:
- Check the symptoms you have and examine the breasts.
- Ask questions about your past mastitis infections, sore or cracked nipples, and if the baby latches to the breast correctly.
- If your breast displays a discharge, then the doctor may send a sample to send for laboratory analysis, to detect the presence of pathogens.
If the diagnosis of mastitis is positive, the doctor would suggest the treatment options for it.
How Is Mastitis Treated?
Mastitis is treated through the following steps and measures:
- Emptying the breast periodically: The best way to drain the breasts is to let the infant breastfeed. But if your baby is unable to breastfeed properly, then talk to a lactation consultant. The consultant may suggest expressing or pumping breastmilk manually, which is an ideal alternative when suckling is painful.
- Antibiotic course: If the mastitis develops an infection, then you may be prescribed an antibiotic course, usually for 10-14 days, depending on the severity of it (5). Finish the entire course to prevent recurrence. The most commonly prescribed antibiotic for mastitis treatment is Amoxicillin, which is regarded as safe for the lactating infant (6).
However, the doctor may prescribe a different antibiotic keeping in mind the baby’s age, health, and the mother’s overall health.
Expressing milk and using antibiotics can give you relief from pain within two days of treatment. You can expect total relief in about 10-15 days after the treatment begins, although you may have to visit the doctor periodically for followup and to prevent recurrence.
How To Manage Mastitis?
Home care and management are essential to ease the symptoms and successfully treat mastitis. Here is how you can manage mastitis at home:
- Take rest: Drink plenty of fluids and get adequate rest to feel better. Relaxing the body, while periodically draining your breasts, will allow the milk to flow through the nipple smoothly and reduce engorgement too.
- Use a warm compress or ice pack: Apply a warm compress or an ice pack, whichever feels better, to the engorged breast. If you are using an ice pack, then place it over your bra and not directly on the skin.
- Massage breasts gently before feeding: If the inflammation is preventing free-flow of milk, then gently massage the breast in circular strokes to stimulate the movement of milk towards the nipple.
- Wear loose clothing: Choose loose clothing that does not constrict your breasts. Give yourself some time without a bra, to reduce pressure on the breasts.
- Let the nipple air-dry after breastfeeding: Once done with feeding, let the nipple air-dry a bit. It reduces the susceptibility to bacterial contamination due to the residue milk around the nipple.
- Use acetaminophen or ibuprofen for pain: If experiencing pain in the breasts, then take acetaminophen (Tylenol) or ibuprofen (Advil) (6). These medicines are safe to use during breastfeeding. But check the dosage instructions on the label and also consult your doctor before taking these medicines.
Don’t just focus on your baby but take care of yourself too because ignoring mastitis could lead to a more painful complication.
What Are The Complications Of Mastitis?
Untreated mastitis can lead to a breast abscess. A breast abscess is a condition where white blood cells attack the infection-causing pathogen within the organ, eventually causing painful accumulation of pus (7).
Antibiotics are the first line of treatment to cure breast abscess. However, if symptoms do not subside, then lancing of pus is required. An ultrasound is conducted before the operation to determine the extent of the abscess. The minor surgery involves the use of local anesthesia and removal of the pus using a needle or by making an incision.
The incision is usually small and should not interfere with breastfeeding. You are discharged the same day after the procedure and a few hours of observation. If the abscess is too dense, then several minor procedures may be required to remove it entirely.
Antibiotics are prescribed after the operation, and complete relief occurs in a couple of weeks.
How To Prevent Mastitis?
You can prevent mastitis by following the simple steps mentioned below (8):
- Regular breastfeeding or expressing of milk: Maintain a continual breastfeeding schedule with gaps of a few hours between each feed. Letting your breast drain often prevents the accumulation of milk. If, for some reason, you are unable to breastfeed, then make sure to express milk for storage and use later.
- Use both breasts for feeding: Breastfeed the baby from both breasts, but move to the second only after draining the first one completely. This prevents accumulation of breastmilk.
- Consult a lactation expert for latching problems: If your little one does not seem to feed properly due to latching problems, then consult a lactation expert. The consultant can guide you on the best breastfeeding positions that work well with your baby.
- Address sore or cracked nipples quickly: Do not ignore those sore nipples. Medical experts suggest using a lanolin-based cream that heals cracked nipples while also keeping them healthy.
- Avoid ill-fitting bras: Ill-fitting bras and clothes can restrict the flow of milk through the milk ducts, thus causing engorgement. Choose the right fitting attire so that you are not prone to mastitis.
- Wean the infant gradually: When weaning your baby from breastfeeding, make sure to do it slowly. Do not try to stop breastfeeding overnight! Instead, do it gradually by reducing the number of breastfeeds per day. It will help your breasts adjust to the reduced demand for milk and minimize the production.
Keep reading to know the answers to some more commonly asked questions about mastitis.
Frequently Asked Questions
1. Can I get mastitis from pumping?
No. Pumping your breasts reduces the risk of breast engorgement and subsequent mastitis infection. Pumping breast milk will not cause any complications such as pain or sore nipples. If you have pain while pumping, then check for cracked nipples or any other injury to your breast (9).
2. Does mastitis affect milk supply?
Yes. Mastitis can reduce the breast milk supply since the infection affects the milk ducts. However, undamaged milk ducts can compensate and produce extra milk so that your baby does not have a shortage of food (10). Once the breasts begin to heal, all milk ducts resume normal milk production.
3. Can I breastfeed during mastitis?
Yes. Breastfeeding during mastitis is one of the best ways to alleviate its symptoms. Experts state that even if you have infective mastitis, it is okay to feed the baby since your milk will contain antibodies that will protect the baby.
4. Can I feed with breast abscess?
Yes. Breast abscess will not harm the baby, as the pus is too thick to pass through the nipple. Even after surgery, you should not have any problem with breastfeeding, and the doctor will suggest the right method to breastfeed. Experts state that breastfeeding should not cease during breast abscess, as the symptoms of the condition may improve with regular breastfeeding.
5. Can I breastfeed while getting treated for mastitis?
Yes. You will most likely be prescribed antibiotics that are compatible with breastfeeding. However, if you are given something that does not go well with breastfeeding, your doctor will let you know about it, and help you adjust breastfeeding schedule accordingly.
6. Can I get mastitis cured without antibiotics?
Yes, but only if it is non-infective. If there is no infection by a pathogen in the blocked milk ducts, then you can cure mastitis through self-management alone. However, if bacteria infect the blocked milk ducts, then you will need antibiotics (11).
Mastitis during breastfeeding can be a painful experience. But do not stop breastfeeding due to it, as lactating can help soothe the pain and help manage the condition. If you display signs of mastitis, consult your doctor immediately for timely treatment and prevent further complications such as breast abscess, which may require surgical intervention. Since prevention is better than cure, it is advisable to take the necessary measures such as nursing from both the breasts equally, feeding regularly, and avoiding weaning too early to avoid such discomforts.
References
- Mastitis.
https://www.nhs.uk/conditions/mastitis/ - Mastitis.
https://my.clevelandclinic.org/health/diseases/15613-mastitis - Blocked milk ducts and mastitis.
https://www.childrens.health.qld.gov.au/fact-sheet-blocked-milk-ducts-and-mastitis - Periductal mastitis.
https://breastcancernow.org/information-support/have-i-got-breast-cancer/benign-breast-conditions/periductal-mastitis// - Jeanne P. Spencer; (2008); Management of Mastitis in Breastfeeding Women.
https://www.aafp.org/pubs/afp/issues/2008/0915/p727.html - The Transfer of Drugs and Other Chemicals Into Human Milk .
https://publications.aap.org/pediatrics/article-abstract/108/3/776/66674/The-Transfer-of-Drugs-and-Other-Chemicals-Into?redirectedFrom=fulltext - Breast abscess.
https://www.nhs.uk/conditions/breast-abscess/ - Preventing Mastitis.
https://www.uofmhealth.org/health-library/tn8011#tn8011-sec - Injury and Infection.
https://www.fda.gov/medical-devices/breast-pumps/injury-and-infection - Breastfeeding—blocked ducts and mastitis.
https://brochures.mater.org.au/brochures/mater-mothers-hospital/breastfeeding-blocked-ducts-and-mastitis - Mastitis.
https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=85&contentid=P01215
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sharon Somekh
Read full bio of Rohit Garoo